Hong Kong J Psychiatry 2005;15(3):89-96
ORIGINAL ARTICLE
Ho-Wai So, MSc, Department of Clinical Psychology, Kwai Chung Hospital, New Territories Hong Kong, China.
Address for correspondence: Ho-Wai So, Department of Clinical
Psychology, Kwai Chung Hospital, 3-15 Kwai Chung Hospital Road, New Territories, Hong Kong, China.
Tel: (852) 2959 8470; Fax: (852) 2371 3197;
E-mail: sohowai@yahoo.com
Submitted: 5 October 2005; Accepted: 15 March 2006
Abstract
Objective: To examine the Millon Clinical Multiaxial Inventory-III profiles of substance abus- ers and the relationship of these profiles to characteristics of the substance abuse.
Patients and Methods: A sample of 107 Chinese substance abusers in Hong Kong completed the Millon Clinical Multiaxial Inventory-III, the Sensation Seeking Scale (Form V), and a ques- tionnaire on substance use. Analysis was undertaken to determine the most prevalent psychopathologies. Subgroup analysis further evaluated differences between groups on Axis I and II psychopathologies, as well as in the pattern of substance use.
Results: The participants showed elevations on a number of Millon Clinical Multiaxial Inven- tory-III scales. Subgroups were identified using the dimensions of depressive trait and sensation seeking. Comparisons between subgroups revealed systematic differences in Axis I and Axis II scale elevations, as well as in the pattern of substance use.
Conclusions: The findings showed support for both the self-medication and sensation-seeking hypotheses of substance abuse. Further studies are indicated to study the interaction of Axis I and Axis II pathologies and substance abuse, and its clinical implications.
Key words: Chinese, Comorbidity, Personality disorders, Substance abuse
Introduction
Addiction was historically thought to be a symptom of personality disorder (PD). With the advent of the multiaxial Diagnostic and Statistical Manual of Mental Disorders, 3rd edition (DSM-III),1 substance use disorders were defined as a clinical syndrome and separated from personality pathology. Since then, psychiatric comorbidity in substance abusers has been a topic of considerable interest.
In a recent national epidemiological survey conducted in the United States, Grant et al reported the prevalence of substance use disorders as 9.35%, among whom 19.67% had at least 1 independent mood disorder during the same 12-month period.2 Estimates of the prevalence of mood disorders among substance abusers are typically in the range 15-30%.3 McMahon and Davidson found that 66% of male alcoholics undergoing inpatient treatment showed elevation on the Dysthymia scale of the Millon Clinical Multiaxial Inventory (MCMI).4 Ball et al also reported that affective disturbance was the most common (66%) Axis I subtype on the MCMI-III profile for a group of patients with opioid dependence.5 It is difficult to say how much of this psycho- pathology is a function of the substance itself and how much preceded the substance abuse, however. Rounsaville et al addressed this question, comparing the ages of onset of the disorders with the age of first substance use.6 They found that substance abuse more often preceded major and minor depression, mania, and alcoholism, whereas phobias preceded the onset of substance abuse, and generalised anxiety disorder was equally divided between precedent and subsequent development relative to substance abuse.
The median rates for PDs across different studies range from a low of 44% for alcohol-dependent individuals, to a high of 79% for opioid-dependent patients.7 According to a review by Verheul et al,8 Cluster B PDs — Antisocial, Borderline, and less frequently Narcissistic and Histrionic PDs — are the most prevalent. However, both Cluster C (Avoidant and Dependent, and less frequently Obsessive- Compulsive disorder) and Cluster A (Paranoid and less frequently Schizoid and Schizotypal disorders) are also common in treated substance abusers. In a sample of 370 opiate, cocaine, and alcohol-dependent patients, Rounsaville et al found that the majority of substance abusers (70%) met criteria for one or more PDs.9 In that study, Cluster B disorders were the most prevalent (61%), followed by Cluster C (34%) and Cluster A (22%). Antisocial (46%), Border- line (30%), and Avoidant (20%) disorders have been identi- fied as the most common specific PDs.9-11
The co-occurrence of substance abuse and PD has been shown to be associated with greater substance abuse and psychiatric symptomatology,9,10,12 and an increased risk for suicide, hospitalisation, repeated treatment admissions, over- utilisation of medical care, employment and legal problems, victimisation or perpetration of abuse, as well as human immunodeficiency virus infection.13 In addition, the pres- ence of a comorbid PD appears to be associated with failure to complete treatment for substance abuse and poorer treat- ment outcome.14-16 Studies evaluating the match of patient to treatment approach, suggest that the presence of a co- occurring psychiatric disorder indicates the need for spe- cialised or more intensive treatment.17-20
Conversely, it has been argued that biologically influ- enced temperament and personality traits (eg, impulsivity, novelty or sensation seeking) have a central role in addic- tive behaviour. According to Cloninger's psychobiological theory,21 Type 1 personality is characterised as low in nov- elty (sensation) seeking, high in harm avoidance (anxious), and high in reward dependence (dependent), whereas Type 2 personality is high in sensation seeking, low in harm avoid- ance (fearless), and low in reward dependence (autonomous). People with a Type 1 personality tend to consume alcohol to reduce anxiety and distress, whereas those with a Type 2 personality consume alcohol because they enjoy the dis- inhibition it produces. This latter group are more likely to engage in fighting and other antisocial behaviour.
Zuckerman,22 supporting Cloninger's theory, postulated that a tendency to seek out novel and exciting experiences is a factor that increases risk for substance use and other risk-taking behaviour. By engaging in risky behaviour, these individuals seek to increase their unusually low arousal to an optimal level.23 This construct of sensation seeking has been consistently related to substance use and abuse in ado- lescents and adults.11 Higher sensation seeking has been associated with vulnerability to substance use, chronicity of substance dependence, and co-occurring psychiatric disorders.24 The highest sensation seekers are polydrug users, characterised by the number and variety of substances they use concurrently or over their life history, rather than by the particular substances they abuse.25,26
According to the self-medication model of substance abuse as argued by Khantzian, individuals select a substance of choice to provide relief from specific, painful, affective states.27 This model has been supported by studies that found associations between emotional instability and the use of sedatives-hypnotics and alcohol.28-30
Although a number of studies have investigated the re- lationship between PDs and substance use, few studies have examined the full spectrum of PDs among abusers of a wide range of psychotropic substances. Most existing studies ei- ther examined only a few particular PDs (such as Antisocial PD [APD] and Borderline PD28,29), or included participants who abused only a particular type of substance, such as cocaine,25 heroin,31 or alcohol.4 Further, no study to date has evaluated the relationship between PD and substance use among Chinese substance abusers.
The present study is the first to examine PD profiles of Chinese substance abusers in Hong Kong, using the Chi- nese translation of the MCMI-III.
Patients and Methods
Participants
The participants in this study were 107 Chinese substance abusers consecutively admitted to an assessment programme of a substance abuse clinic at a psychiatric hospital in Hong Kong. Diagnoses were made by the treating psychiatrist, based on the DSM-IV criteria for substance use disorders. Patients gave written informed consent. Exclusion criteria were inability to comprehend or complete study procedures, active psychotic symptoms, and presence of organic brain disorder.
The sample had a mean age of 30.72 years (SD 11.30), with a range from 16 to 54 years. About 67% (n = 71) of participants were men. Male participants were generally older than their female counterparts (t = 2.64, p < 0.05). Mean years of formal education for the sample as a whole was 8.43 years (SD 2.29). About 60% of the sample was single, 26.2% were married/living with a partner; and 13.1% were separated/divorced. With respect to occupation, 25.7% worked as unskilled labour; 16.2% as skilled labour or professionals; 8.6% were students; 8.6% were house- wives; and 41% were unemployed. Thus, this sample represented a socially impoverished community in the lower socioeconomic strata. However, the sample group appeared typical of participants in the assessment programme.
Assessment Tools
Personality disorder variables
The MCMI-III32 is a popular instrument for assessment of DSM-IV33 PDs and clinical syndromes. This 175-item self-report inventory consists of 24 clinical scales. The first 14 clinical scales evaluate Millon's Basic and Severe PDs. These scales are a superset of the DSM-IV Axis II PDs. The remaining 10 scales evaluate Basic and Severe Clinical Syndromes (ie, Axis I disorders). A base rate (BR) score of 85 or above on a scale signifies the "most prominent" disorder, whereas a BR score of 75 or above reflects the "presence of characteristics" of the disorder.
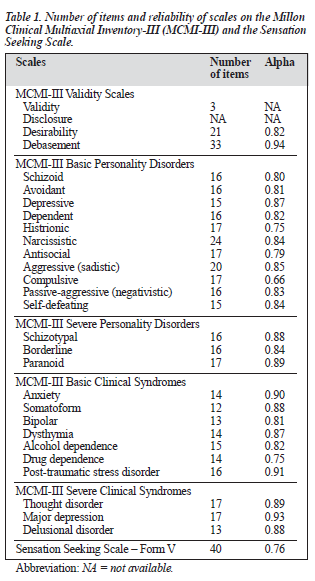
The MCMI-III used in the present study was a recently revised Chinese version. In order to validate the translation, the Chinese version had been back-translated into English. Table 1 presents the number of items and Cronbach alpha (a) reliability coefficient of each scale of this Chinese version. Of the 107 recruits in the study, 100 completed the MCMI-III.
Substance use variables
Substance use variables were measured using a self-report questionnaire designed by the author. Respondents were asked to indicate the substance or substances they had used, the years when they began and stopped using each substance, and the frequency and amount of use. They were also asked to indicate their reasons for substance use. In addition, drug dependence and alcohol dependence were also measured using the MCMI-III Scales T and B, respectively.
Sensation seeking variables
The Sensation Seeking Scale - Form V34 (SSS) was used to assess sensation seeking. This is a 40-item self-report ques- tionnaire that yields scores on a general scale and on four factors: Thrill and adventure seeking; Experience seeking; Disinhibition; and Boredom susceptibility. This widely used scale is considered the standard means of assessing this trait. The SSS was translated into Chinese specifically for the present study. The reliability of this Chinese version was assessed to be satisfactory (see Table 1). Of the 107 recruits into the study, 86 completed the SSS.
Statistical Analysis
All statistics were computed using the Statistical Package for the Social Sciences 9.0 for Windows. Comparisons on continuous variables were assessed with t test analyses (for two-group comparisons) or one-way analysis of variance (ANOVA) for multiple-group comparisons. Analysis of covariance (ANCOVA) was used for group comparisons to determine the linear effect of covariates on the depen- dent variables. When the covariates did not show a linear relationship with the dependent variables, partial cor- relation was completed instead. Categorical variables were analysed using the Chi-squared test, with Yate's correction when appropriate.
Only valid MCMI-III profiles were included in the sub- sequent analyses. MCMI-III profiles were considered valid if the Validity index was > 1, or Scale X < BR 34 or > raw score 178.32 There were four invalid MCMI-III profiles in the sample.
Results
Substance Use Pattern
Table 2 presents the substance use pattern of the sample. Overall, the mean number of drug types used was 2.89 (SD 2.27), ranging from 1 to 13. The mean age of first drug use was 19.2 years (SD 8.16 years), ranging from 9 to 46 years. The mean duration of drug use was 10.36 years (SD 8.00), ranging from 1 to 35 years.
There was no statistically significant difference between men and women in the sample with respect to number of drug types used, age of first use, duration of substance use, substance of primary use, substance of secondary use, frequency of drug use, or primary reason for drug use.
Among the 106 participants who reported the type(s) of substance they had used, 69 reported use of more than one substance. In general, the majority of participants (57%) reported that their problem drugs were heroin alone or in com- bination with other drugs. Fifteen percent reported that their problem drugs were amphetamines alone or in combination with other drugs. Of the secondary drugs used, 19.6% were tobacco, 12.2% heroin or methadone, and 10.3% cannabis.
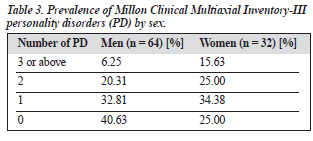
Prevalence of Axis II Personality Disorders
The prevalence of PDs, as assessed by the MCMI-III is shown in Table 3. About 65% of all participants scored 85 or above on one or more of the MCMI-III PD scales. The average number of PDs was 1.02 (SD 11.25) for men and 1.41 (SD 1.21) for women. There was no significant differ- ence between men and women in the prevalence rates for PD or the mean number of PDs.
Most of the MCMI-III PD scales were elevated, ex- cept for the Histrionic PD and Compulsive PD scales. The scales that had the highest mean BR scores were APD (73.65, SD 11.78), Self-defeating PD (72.28, SD 13.99), Dependent PD (70.71, SD 16.71), and Depressive PD (69.66, SD 22.27). APD correlated positively with alcohol dependence (r = 0.58, p < 0.01), drug dependence (r = 0.61, p < 0.01) and type of drugs used (r = 0.21, p < 0.05), and was correlated negatively with age of first substance use (r = -0.29, p < 0.01).
Prevalence of Axis I Clinical Syndromes
Subgroup Comparisons
In order to identify qualitatively different subgroups of sub- stance abusers, a Depressive trait dimension was computed (Cronbach a = 0.81). To minimise item overlap across MCMI scales, this new dimension included only the eight prototypic items from the Depressive PD scale. The substance abusers were divided into two groups by the median score on this dimension.
Depressive versus non-depressive substance abusers
Comparisons were made of MCMI-III Axis I psycho- pathology for depressive versus non-depressive substance abuser subgroups. Substance abusers with high depres- sive trait scored significantly (p < 0.01) higher than their counterparts with low depressive trait on the following MCMI-III clinical syndrome scales: Anxiety (t = 6.50), Somatoform (t = 3.05), Bipolar (t = 3.62), Dysthymia (t = 5.58), Post-traumatic stress disorder (PTSD; t = 8.58), Thought disorder (t = 4.34), Major depression (t = 5.44), and Delusional disorder (t = 3.17). As shown by their higher scores on the Disclosure (t = 8.30, p < 0.01) and Debasement (t = 8.62, p < 0.01) scales, and lower scores on the Desirability scale (t = -5.62, p > 0.01), substance abusers with high depressive trait appeared to be more likely to report psychopathology.
In order to examine the possible impact of mood state on the relationship between depressive trait and clinical syndromes, a partial correlation was performed controlling for the Major depression BR score. After controlling for Major depression, the Depressive trait dimension was still significantly correlated with all the above-mentioned clini- cal syndrome scores (p < 0.05).
Subgroup comparisons on Millon Clinical Multiaxial Inventory-III Axis II personality disorder profile
Compared with low scorers, substance abusers with high depressive trait scored higher on the following PD scales: Schizoid PD (t = 2.51, p < 0.05), Avoidant PD (t = 4.31, p < 0.01), Dependent PD (t = 3.42, p < 0.01), Aggressive PD (t = 2.85, p < 0.01), Passive-aggressive PD (t = 3.38, p < 0.01), Self-defeating PD (t = 3.06, p < 0.01), Schizo- typal PD (t = 3.48, p < 0.01), Borderline PD (t = 4.37, p < 0.01), and Paranoid PD (t = 3.36, p < 0.01). Controlling for Major depression, the Depressive trait dimension correlated positively with all the above-mentioned PDs except for Schizoid and Passive-aggressive PDs (p < 0.05). The correlation was negative between Depressive trait and the following scales: Histrionic PD (r = -0.35, p < 0.01), Narcissistic PD (r = -0.40, p < 0.01), and Compulsive PD (r = -0.24, p < 0.05).
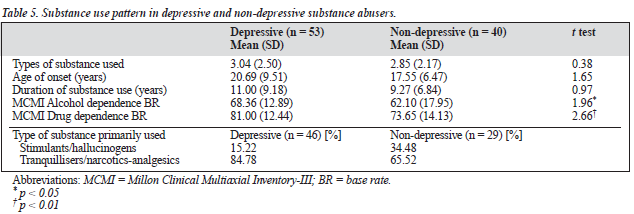
Subgroup comparisons on substance use pattern
As shown in Table 5, substance abusers with high or low depressive trait did not differ in terms of type of substance used, age of first use, and duration of use. However, there was a small, significant group difference in the substance of primary use. In addition, ANCOVA showed that sub- stance abusers with high and low depressive trait differed in Drug dependence (F [1, 90] = 7.04, p < 0.01) and Alcohol dependence (F [1, 90] = 4.00, p < 0.01) even when controlling for Major depression.
One-way ANOVA showed that the two groups differed significantly in the reason given for substance use (F [2, 68] = 4.72, p < 0.05). Specifically, post-hoc analyses found that those who reported "relief from negative mood" as their reason for drug use, scored higher on the depressive trait dimension than those who attributed their substance use to "sensational excitement" (d = 1.69, p < 0.05) or "influence from peer/spouse" (d = 1.70, p < 0.01). ANOVA showed that such group differences remained significant even after controlling for Major depression (F (2, 67) = 6.92, p < 0.01).
High sensation seeking versus low sensation seeking
To study the relationship between sensation seeking, MCMI-III profile and substance use, the sample was divided into two groups according to general score on the SSS.
Comparisons of the two groups were made on MCMI- III Axis I psychopathology. In general, the profile of clinical syndrome scales was elevated for high sensation seekers compared with low sensation seekers. These dif- ferences reached significance on the following scales: Bipolar disorder (t = 3.31, p < 0.01), PTSD (t = 2.20, p < 0.05), and Major depression (t = 2.18, p < 0.05).
Comparisons of the two groups on the MCMI-III Axis II PD profile found the profiles were largely similar. Exceptions were that the high sensation seekers scored significantly higher on Borderline PD (t = 2.28, p < 0.05), whereas the low sensation seekers scored higher on Compulsive PD (t = -3.86, p < 0.01).
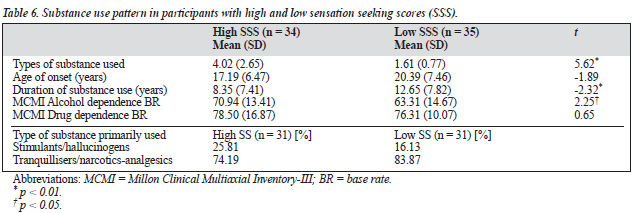
Comparison of high and low sensation seeking groups on substance use pattern
The substance use pattern for participants with high and low sensation seeking scores is presented in Table 6. High sensation seekers had abused drugs for a significantly shorter period of time and used significantly more types of substances than low sensation seekers. They also scored significantly higher than low sensation seekers on the MCMI-III Alcohol dependence scale. However, the group difference in age of first use and drug dependence was not statistically significant.
There was no significant difference in reported types of substance primarily used by high and low sensation seekers. One-way ANOVA was conducted to examine the relation- ship between the sensation seeking dimension and the reported reason for substance use. There was a significant difference in sensation seeking score across substance abusers reporting various reasons for drug use (F [2, 55] = 3.98, p < 0.05). Specifically, post-hoc comparisons found that those who reported "sensational excitement" as their reason for substance use scored higher on the SSS than those who attributed their substance use to "relief from negative mood" (d = 5.15, p > 0.05), or to "influence from peer/spouse" (d = 5.45, p < 0.05).
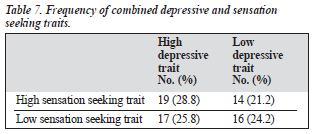
Table 7 presents the frequency and percentage of participants falling into the high and low groups of the depressive trait dimension and sensation seeking dimension. The two trait dimensions separated the sample into four rather evenly distributed groups. Cluster analysis could not be performed due to the small sample size of each group.
Discussion
The present study had a number of interesting findings. Specifically, it showed that:
- Chinese substance abusers had a high prevalence of Axis I and Axis II disorders;
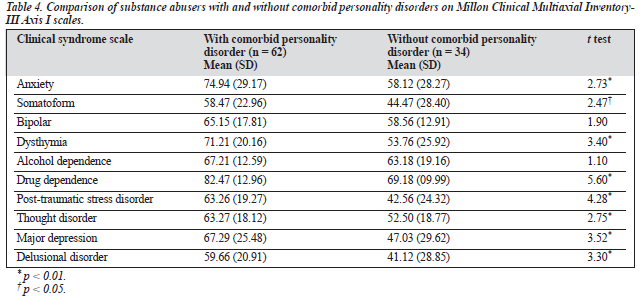
- substance abusers with comorbid PDs had more severe psychopathology than those without comorbidities;
- the depressive substance abusers scored higher than the non-depressive group on many of the Axis I and Axis II scales. Such group differences were attributed to the depressive trait, rather than the depressive mood state;
- the depressive subjects had a more severe substance use profile, tended to abuse tranquillisers/narcotics-analgesics, and to abuse drugs for the purpose of "self-medication";
- high sensation seekers had a different profile of Axis I and Axis II disorders from low sensation seekers; and
- high sensation seekers tended to use a diverse range of substances, to have a shorter duration of substance use, and to use substances for "sensational excitement".
Consistent with previous findings,10,11 APD was the most prevalent single PD in the present sample, and equally pre- valent in the depressive and non-depressive subgroups. In keeping with the findings of Cecero et al,12 APD was associated with more severe drug and alcohol dependence, earlier onset of substance use, and a more diverse choice of drugs.
The profile of Axis I scale elevations implicated prob- lems of mood dysregulation in the present sample of sub- stance abusers. Such problems were more marked among participants with a high depressive trait. As suggested by the "self-medication hypothesis", these depressive substance abusers tended to use drugs that have calming, hypnotic, and pain relief functions. It is likely that these substance abusers chose the drugs for their psychopharmacological properties, so as to cope with distressful subjective states and an external reality otherwise experienced as un- manageable. Alternatively, the positive correlation between depressive trait and age could suggest that mood problems may emerge with social withdrawal and feelings of iso- lation after prolonged drug dependence. This is consistent with the finding that the depressive subgroup showed a more severe Cluster A (ie, Paranoid, Schizoid and Schizotypal PDs) and Cluster C (ie, Avoidant and Dependent PDs) profile.
The Axis I and Axis II profile of high sensation seekers in this study was characterised by low socialisation, high impulsivity, irritability, non-conformity and recklessness. In keeping with previous findings,25,35-37 the high sensation seekers were attracted to stimulants, as well as to depressants, tranquillisers and narcotics. As suggested by the sensation seeking hypothesis, these individuals were attracted to sub- stances that alter their state of consciousness, regardless of the psychopharmacological properties of the drugs.
Sensation seeking was negatively associated with the duration of drug use. This is consistent with the findings of Spotts and Shontz,38 where the more chronic drug users tended to be less sensation seeking. It seems likely that individuals, especially adolescents, begin to use drugs for the sensational excitement, and thus try a variety of dif- ferent substances. However, after some years of addiction, they are no longer looking for novel experiences from the substance. Rather, chronic substance users fixate on one drug that they are most dependent on and seek to use the drug in order to avoid withdrawal effects and to relieve negative affective states, such as anxiety and depression. This hypothesis is supported by the fact that in the present sample, age was negatively correlated with the SSS score, yet positively correlated with major depression and depres- sive PD score.
The findings in this study shed light on the relationship between Axis I and Axis II disorders and patterns of sub- stance abuse. The present results find support for both the self-medication and sensation-seeking hypotheses of sub- stance abuse. Assessment of personality profile is of impor- tance in understanding the aetiology of substance abuse and in improving the patient-treatment match. The present study is limited by a relatively small sample size, however. In addition, the variables assessed in this study were based on self-report measures, rather than clinician ratings. The reliability of retrospective self-report of substance use is uncertain. Further studies, with a larger sample and more comprehensive assessment measurements, are indicated to study the interaction of Axis I and Axis II pathologies on substance abuse, using more sophisticated statistical analy- sis methods, such as path models or multivariate analyses.
References
- Ball SA, Nich C, Rounsaville BJ, Eagan D, Carroll KM. Millon Clini- cal Multiaxial Inventory-III substypes of opioid dependence: Validity and matching to behavioral therapies. J Consult Clin Psychol 2004;72: 698-711.
- Rounsaville BJ, Anton SF, Carroll K, Budde D, Prusoff D, Gawin F. Psychiatric diagnosis of treatment-seeking cocaine abusers. Arch Gen Psychiatry 1991;48:43-51.
- Ball SA. Personality traits, problems, and disorders: Clinical applica- tions to substance use disorders. J Res Pers 2005;39:84-102.
- Verheul R, van den Brink W, Hartgers C. Prevalence of personality disorders among alcoholics and drug addicts: an overview. Eur Addict Res 1995;1:166-177.
- Rounsaville BJ, Kranzler HR, Ball S, Tennen H, Poling J, Triffleman E. Personality disorders in substance abusers: Relation to substance use. J Nerv Ment Dis 1998;186:87-95.
- Brooner RK, King VL, Kidorf M, Schmidt CW, Bigelow GE. Psychi- atric and substance use comorbidity among treatment-seeking opioid abusers. Arch Gen Psychiatry 1997;54:71-79.
- Zuckerman M. Vulnerability to psychopathology: A biosocial model. Washington, DC: American Psychological Association; 1999.
- Cecero JJ, Ball SA, Tennen H, Kranzler HR, Rounsaville BJ. Concur- rent and predictive validity of antisocial personality disorder subtyping among substance abusers. J Nerv Ment Dis 1999;187:478-486.
- Target M. Outcome research on the psychosocial treatment of person- ality disorders. Bull Menninger Clin 1998;62:215-230.
- Griggs SM, Tyrer PJ. Personality disorder, social adjustment and treat- ment outcome in alcoholics. J Stud Alcohol 1981;42:802-805.
- Nace EP, Davis CW. Treatment outcome in substance abusing patients with a personality disorder. Am J Addict 1993;2:26-33.
- Thomas VH, Melchert TP, Banken JA. Substance dependence and per- sonality disorders: Comorbidity and treatment outcome in an inpatient treatment population. J Stud Alcohol 1999;60:271-277.
- Cacciola JS, Rutherford MJ, Alterman AI, McKay JR, Snider EC. Per- sonality disorders and treatment outcome in methadone maintenance patients. J Nerv Ment Dis 1996;184:234-239.
- Carroll KM, Rounsaville BJ, Gordon LT, et al. Psychotherapy and phar- macotherapy for ambulatory cocaine abusers. Arch Gen Psychiatry 1994;51:177-187.
- McLellan AT, Luborsky L, Woody GE, O'Brien CP, Druley KA. Pre- dicting response to alcohol and drug abuse treatments: Role of psychi- atric severity. Arch Gen Psychiatry 1983;40:620-625.
- Messina N. Farabee D, Rawson R. Treatment responsivity of cocaine- dependent patients with antisocial personality disorder to cognitive- behavioral and contingency management interventions. J Consult Clin Psychol 2003;71:320-329.
- Cloninger CR. Neurogenic adaptive mechanisms in alcoholism. Science 1987;236 410-416.
- Zuckerman M. Behavioural expressions and biosocial bases of sensa- tion seeking. New York: Cambridge University Press; 1994.
- Zuckerman M. A biological theory of sensation seeking. In: Zuckerman M, editor. Biological bases of sensation seeking, impulsivity, and anxiety. Hillsdale, NJ: Erlbaum;1983:37-76.
- Ball SA. Big five, alternative five, and seven personality dimensions: Validity in substance dependent patients. In: Costa PT Jr, Widiger TA, editors. Personality disorders and the five-factor model of personality. 2nd ed. Washington, DC: American Psychological Association; 2002.
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. Washington, DC: American Psy- chiatric Press; 1980.
- Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occur- rence of substance use disorders and independent mood and anxiety disorders. Arch Gen Psychiatry 2004;61:807-816.
- Kranzler HR, Rounsaville BJ. Dual diagnosis and treatment: Substance abuse and comorbid medical and psychiatric disorders. New York: Marcel Dekker, Inc; 1998.
- McMahon RC, Davidson RS. An examination of depressed vs. non- depressed alcoholics in inpatient treatment. J Clin Psychol 1986;42: 177-184.
- Ball SA, Carroll KM, Rounsaville BJ. Sensation seeking, substance abuse, and psychopathology in treatment-seeking and community co- caine abusers. J Consult Clin Psychol 1994;62:1053-1057.
- Kern MF, Kenkell MB, Templer DI, Newell TG. Drug preference as a function of arousal and stimulus screening. Int J Addict 1986;21: 255-265.
- Khantzian EJ. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. Am J Psychiatry 1985;142: 1259-1264.
- Dulit R, Fyer M, Haas G, Sullivan T, Frances A. Substance use in bor- derline personality disorder. Am J Psychiatry 1990;147:1002-1007.
- Hatzitaskos P, Soldatos CR, Kokkevi A, Stefanis CN. Substance abuse patterns and their association with psychopathology and type of hostility in male patients with borderline and antisocial personality disorder. Compr Psychiatry 1999;40:278-282.
- Mirin SM, Weiss RD. Substance abuse and mental illness. In: Frances RJ, Miller SI, editors. Clinical textbook of addictive disorders. New York, NY: Guildford; 1991.
- Patalano F. Cross-cultural similarities in the personality dimensions of heroin users. J Psychol 1998;132:671-673.
- Millon T. Millon Clinical Multiaxial Inventory Manual. 3rd edition. Minneapolis, MN: National Computer Systems; 1994.
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Press; 1994.
- Zuckerman M. Sensation Seeking: Beyond the Optimal Level of Arousal. Hillsdale, NJ: Erlbaum; 1979.
- Craig RJ. Personality characteristics of heroine addicts: Review of empirical research 1976-1979. Int J Addict 1982;17:227-248.
- Craig RJ. The personality structure of heroin addicts. NIDA Res Monogr 1986;74:25-36.
- Teichman M, Barnea Z, Rahav G. Sensation seeking, state and trait anxiety, and depressive mood in adolescent substance users. Int J Addict 1989;24:87-99.
- Spotts JV, Shontz FC. Correlates of sensation seeking by heavy chronic drug users. Percept Mot Skills 1984;58:427-435.