Hong Kong J Psychiatry 2005;15(3):97-100
ORIGINAL ARTICLE
Dr Jitendra K Trivedi, MD (Psych), MRCPsych (UK), Professor, Department of Psychiatry, King George's Medical University, Lucknow, India. Dr Sachin Sharma, MBBS, MD (Std), Department of Psychiatry, King George's Medical University, Lucknow, India.
Dr Anand P Singh, PhD, Former Research Associate, Department of Psychiatry, King George's Medical University, Lucknow, India.
Mr Pramod K Sinha, MSc, DSQC, Statistician, Department of Psychiatry, King George's Medical University, Lucknow, India.
Dr Rajul Tandon, MD, Former Research Associate, Department of Psychiatry, King George's Medical University, Lucknow, India.
Address for correspondence: Professor Jitendra K Trivedi, Department of Psychiatry, King George's Medical University, Lucknow, India.
Tel: (91 522) 265 1173; Fax: (91 522) 226 0173;
E-mail: jktrivedi@hotmail.com
Submitted: 2 October 2005; Accepted: 15 March 2006
Abstract
Objective: To assess for the presence of cognitive deficits in patients with somatisation disorder.
Patients and Methods: Twenty patients meeting International Classification of Diseases-10 criteria for somatisation disorder were assessed using computer-based cognitive tests for executive functions (Wisconsin Card Sorting Test, attention and vigilance performance on the Continuous Performance Test, and spatial working memory on the Spatial Working Memory Test). Fifteen controls (matched by age, education and sex) were also assessed.
Results: The patient group's performance was impaired on the Wisconsin Card Sorting Test compared with the control group. Performance on tests of attention and concentration was also significantly worse in the patient group. On the Spatial Working Memory Test, a significant difference was found on delayed retrieval but not on immediate recall.
Conclusion: Patients with somatisation disorder may have objective cognitive deficits. Potential enduring deficits in areas of executive function, attention, concentration and memory may contribute to poor psychosocial functioning.
Key words: Attention, Cognitive aspects, Memory, Neuropsychological tests, Somatization disorder
Introduction
Somatoform disorders are a broad group of illnesses that encompass mind-body interactions in which the percep- tion of bodily complaints cannot be adequately explained through physical deficits. Somatisation disorder is a spe- cific somatoform disorder characterised by a multiplicity of bodily complaints, with multiple organ systems affected, and accompanied by psychopathological (eg, depression and anxiety) and neuropsychological symptoms.1 Neuro- psychological studies have attempted to describe cognitive functioning and to clarify the relationships between cogni- tive complaints and cognitive performance in a wide range of psychiatric disorders. However, there has been limited research on cognitive function in somatoform disorders compared with studies in other psychiatric disorders.2 It has been suggested that patients with somatization disorder may suffer from substantial problems in cognitive performance.3 Although the range of cognitive problems can be quite di- verse, certain cognitive domains such as executive function, attention-vigilance and memory appear to be more at risk in psychiatric disorders ranging from schizophrenia to obsessive-compulsive disorder.
This preliminary study attempts to describe the cognitive function of patients with somatisation disorders. Executive function, attention-vigilance working memory were studied. Executive function refers to the ability to use high-level over- sight functions to modulate memory, sensory information, and affect as a situation evolves and strategies must shift to maintain performance. Aspects of attention and memory5 evaluated were working memory, selective/focused and sustained attention, attentional flexibility, supervisory attentional control, processing speed, learning and retrieval, interference effects and incidental learning. The study aimed to validate patient cognitive complaints from an objective dimension, which may help to identify the under- lying biological basis for these somatic complaints. Among different somatoform disorders, the diagnosis of somatisa- tion disorders seems to have the highest reliability, validity and stability, hence the study included only patients with somatisation disorder to avoid diagnostic controversy.
Patients and Methods
Participants
Patients were screened at outpatient clinics of the Depart- ment of Psychiatry, King George's Medical University, Lucknow, India. Twenty patients satisfying criteria for so- matization disorder diagnosed by using the International Classification of Diseases (ICD)-10 classification6 were Table 1. Results of the Wisconsin Card Sorting Test.
recruited. Other inclusion criteria were as follows: all the patients were aged from 18-55 years, had at least 8 years of formal education, and gave informed consent. Subjects with other significant psychiatric diagnoses (according to ICD- 10), major medical or neurological illnesses, head injury or significant recent or past alcohol or substance abuse were excluded from the study. All patients were using medica- tions at the time of recruitment into the study. Potential sub- jects were interviewed by a psychiatric resident doctor, and their medical records reviewed if indicated. A consultant psychiatrist then audited the first phase results and confirmed the diagnosis. Only patients who received a diagnosis of somatisation disorder from both investigators were included.
Fifteen normal controls, matched to the patient group according to age, gender and education, were chosen from accompanying relatives and friends of the patients so that they were comparable with respect to socioeconomic status. The control group were then subjected to the same exclusion criteria, with the further addition of past history of psychiatric illness and history of psychiatric illness in a first- degree relative as exclusion criteria. All the control group had a score of 3 or less on the General Health Questionnaire,7 indicating no major health concerns.
Cognitive assessments
Both the patients and control subjects were then assessed on computer-based tests including the Wisconsin Cord Sorting Test (WCST),8 computer version 2, the computer ver- sion of the Continuous Performance Test (CPT),9,10 and the Spatial Working Memory Test (SWMT), number 8 V2.0.11 No benzodiazepines had been taken on the morning of the assessment. The tests were performed between 10 am to 2 pm, thus minimising confounding factors of drowsiness or withdrawal symptoms.
Statistical analysis
The cognitive test scores obtained from the patients and controls were compared using the Student's t test (two-tailed). A p value of < 0.05 was considered statistically significant.
Results
A total of 20 patients with somatisation disorder and 15 controls satisfied inclusion criteria for the study and were recruited. The patient group (n = 20) had a mean age of 34.98 years (SD 10.63), a mean educational level of 11.9 years (SD 3.61) and 82% were males. The control group (n = 15) had a mean age of 34.26 years (SD 11.11), a mean educational level of 10.8 years (SD 2.49) and 80% were males. There was no statistically significant difference between the two groups on these demographic variables.
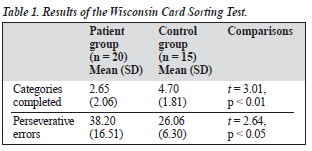
The results on the WCST for the two groups are pre- sented in Table 1. The mean differences between the two groups in terms of both categories completed and number of perseverative errors were found to be statistically signifi- cant. Control subjects completed more categories and committed less perseverative errors on the WCST, compared with patients.
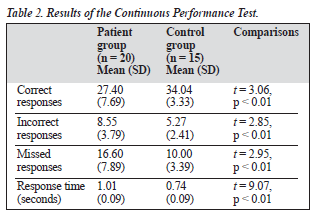
Various parameters of the CPT were compared between the patient and control groups. These data are reported in Table 2. The mean differences show that patients responded correctly less often, committed more errors, had more missed responses and also took longer to respond than controls on this test.
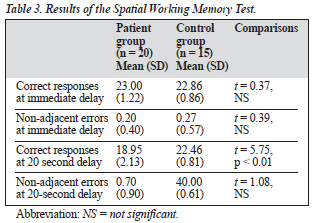
Table 3 shows results on the SWMT for the two groups at immediate delay (zero-second delay) and 20-second delay. At immediate delay, no significant difference in performance between the patient and control groups was observed. At a 20-second delay, the patient group made significantly fewer correct responses than the control group, although no significant difference between the groups was observed for non-adjacent errors.
Discussion
The cognitive performance of patients with somatization disorder but without other Axis-I psychiatric illness was explored. The study compared executive function, spatial working memory and attention-concentration abilities of individuals with somatisation disorder with that of matched controls. Attention-concentration abilities and spatial work- ing memory were found to be relatively impaired in the patient group compared with controls. When attention- concentration abilities were assessed using the computer version of the CPT,9,10 the patient group was found to make fewer correct responses, more incorrect and missed res- ponses, and had a longer response time than controls.
A pilot study by Niemi et al evaluating performance on these same variables also reported that patients with somatisation disorder performed significantly worse than healthy controls.3 These findings suggest that patients with different somatic symptoms perform worse on visuo- motor search tasks than controls. However, it should be noted that poor performance (more errors, slow reactions) alone is not considered proof of poor sustained attention. The essential point is to evaluate whether subjects maintain their original level of performance.12 Some studies have reported no significant differences with regard to rate of increase in error scores or reaction time (performance decrement) be- tween patients with somatisation disorder and healthy controls. On pursuit tracking tasks however, patients with somatisation disorder have been found to show significantly more fluctuation in tracking performance compared with healthy controls.2
For spatial working memory assessed using the com- puter version of the SWMT,11 patients with somatisation disorder again showed a differing pattern from controls. Although patients performed significantly worse than controls at a 20-second delay on this test, no significant difference was noted between the patient and control groups at immediate (0-second) delay. Also, at a 20-second delay, no significant differences were seen between the two groups with respect to non-adjacent errors.
Executive function was assessed using the computer version of the WCST.8 The present study found that patients with somatisation disorder completed fewer cate- gories and committed more perseverative errors than did controls. Executive function has been investigated in earlier studies, and the view expressed that cognitive dysfunction in patients with somatisation disorder may be related to
Neurocognition in Somatisation Disorder
with most notable impairment in verbal memory and visuo- spatial skills, and a slower performance on attentional tasks demanding working memory and sustained vigilance. The pilot study included only a limited sample size and the results of the study may not be generalisable.
Deficient performance within these cognitive domains has important clinical implications, including employability, social competency and successful independent living. For example, tests of attention and executive function measure flexibility of thinking, the ability to switch conversational topics without difficulty and to make decisions without being immobilised. These mental skills are necessary to carry out even routine daily activities. Moreover, attention is necessary whenever an individual is to complete goal- oriented tasks. However, the results of the present study should be interpreted with the limitations of the study.
The major limitation of this study was the small sample size and inability to address potential confounding factors. The effect of medications (antidepressants and benzodia- zepines) on cognitive function is controversial, as studies have shown conflicting results.14,15 The study was completed in an outpatient setting, without a stringent research protocol. The study was cross-sectional; however, to further clarify the state versus trait controversy, longitudinal studies are needed. Another limitation of the study was the omission of a global cognitive test. Other cognitive domains (eg, language) were not assessed. Reports of specific cognitive tests can make it difficult to interpret findings in light of a comprehensive cognitive profile.
Nevertheless, our results suggest that somatization dis- order is accompanied by a range of cognitive impairments. The present article draws attention to the relationship be- tween somatization disorder and cognitive performance. Cognitive problems in severe somatization disorder provide a challenge to future research, as well as to clinical diagnosis and treatment. Current data suggest, that slowed processing speed, impaired working memory, poor learning of new information, poor set shifting and planning ability may be features of cognitive dysfunctioning in patients with somatisation disorder. The early identification of these dys- functions and further research involving other cognitive functions in a large patient sample would enable appropri- ate advice to be formulated and could provide considerable benefit to patients.
References
impaired anterior control of attention and memory.3,13 Findings suggest that patients with somatisation disorders are unable to discard irrelevant stimuli and may become over- whelmed by this information, similar to what has been proposed to occur in patients with obsessive-compulsive disorder.4
The present study shares many of the findings of the pilot study by Niemi et al.3 Niemi et al reported that pa- tients with somatisation disorder were inferior to controls in performance on several but not all cognitive domains,
Hong Kong J Psychiatry 2005, Vol 15, No.3
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed, text revision. Washington: American Psychiatric Association; 2000.
Williams JM, Watts FN, Macleod C, Mathews A. Cognitive psy- chology and emotional disorders. 2nd ed. Chichester: John Wiley & Sons Ltd; 1997.
Niemi PM, Portin R, Aalto S, Hakala M, Karlsson H. Cognitive functioning in severe somatization — a pilot study. Acta Psychiatr Scand 2002;106:461-463.
Okasha A, Rafaat M, Mahallawy N, et al. Cognitive dysfunction in obsessive-compulsive disorder. Acta Psychiatr Scand 2000;101: 251-255.
99
JK Trivedi, S Sharma, AP Singh, et al
- Cohen RA. The neuropsychology of attention. NewYork: Plenum Press; 11. McGurk SR, Green MF. Simple Spatial Memory Test (8) - V 2.0.
- Developed at the CPN laboratory of the UCLA Clinical Research
- World Health Organization. ICD-10 Classification of Mental and Behavioural Disorder: Clinical Description and Diagnostic Guidelines.
Geneva: World Health Organization; 1992
- Goldberg D, McDowell I, Newell C. Measuring Health: A guide to rating scales and questionnaire. 2nd ed. New York: Oxford University Press; 1972;181:225-236.
- Revonsuo A, Portin R. CogniSpeed®: The computer based measure- ment of cognitive processing. AboaTech Ltd, University of Turku, Turku, Finland, 1995.
- Conners CR. The Continuous Performance Test: Use as a diagnostic tool and measure of treatment outcome. Paper presented at the Annual Meeting of the American Psychological Association, Los Angeles, USA; 1994.
- Mukundan CR. Continuous Performance Test (Computer version). National Institute of Mental Health and Neurosciences, Bangalore. 2001
Centre for the Study of Schizophrenia, 2001.
- Van Zomeren AH, Brouwer WH. Assessment of attention. In: Crawford JR, Parker DM, MkKinlay WW, editors. A handbook of neuropsycho- logical assessment. Hove, UK: Lawrence Earlbaum Associates; 1992: 241-266.
- Stuss DT, Shallice T, Alexander MP, Picton TW. A multidisciplinary approach to anterior attentional function. Ann N Y Acad Sci 1995;769: 191-211.
- Lader M, Bhanj S. Physiological and psychological effects of antide- pressants in man. In: Hoffeneister F, Stille G, editors. Psychotropic agents. Part I: Handbook of experimental pharmacology. New York: Springer-Verlag; 1980, Vol. 55.
- Heaton RK, Crowley TT. Effects of psychiatric disorder and their
somatic treatment or neuropsychological test results. In: Filskov SB, Bou TJ, editors. Handbook of clinical neuropsychology. New York: John Wiley & Sons Ltd. 1981;1:481-525.
100 Hong Kong J Psychiatry 2005, Vol 15, No.3