J.H.K.C. Psych. (1993) 3, Spl, 13-16
ORIGINAL PAPER
SUMMARY
The syndrome of hyperkinetic disorder overlaps with conduct disorder in a substantial degree, and the children suffer from these conditions also have associated problems in academic and reading performance, non-compliance and relationship with people. The Ngau Tau Kok Day Hospital Hyperkinetic Group Treatment offers a comprehensive, multidisciplinary and multimodal approach for the assessment and treatment of this group of children and their parents. On completion of the programme, there is improvement in the parent’s perception of their children behavioual problem but only equivocal result from the teacher’s perspective.
INTRODUCTION
The syndrome of hyperkinetic disorder has stirred up some controversies. The central feature of the hyperkinetic syndrome are inattention, impulsively and hyperactivity. In DSM III, the Attention Deficit Disorder with Hyperactivity (ADDH) requires the presence of all three. In DSM III R the Attention Deficit Hyperactivity Disorder (ADHD) is defined by a list of 14 behavioural criteria (8 out of the 14). It in fact broadened the concept as it is possible that only 2 of the core concept be present. In ICD10, only inattention and hyper-kinesis is required. The ICD 10 definition would require :
- Early onset.
- Combination of overactive, poorly modulated behaviour with marked inattention and lack of persistent task involvement.
- Pervasiveness over situations and persistence over time.
It is also known that there is an overlap with conduct disorder. In fact, to most British psychiatrist, the American concept of ADHD corresponds more to conduct disorder. The co-occurrence of hyperkinesia and conduct disorder often point to a poorer prognosis.
These hyperkinetic children has associated problem in reading difficulties and academic underachievement, non-compliance, poor relationship with adults and peers, and conduct problems. Richman (1982) discovered that a complaint of overactivity in preschool children in fact predicts later antisocial behaviour. Local experience (LUK, 1989 & 1991) suggested that hyperkinetic behaviour in preschool children would develop aggressive and conduct behaviour in middle childhood and possibly personality/ conduct disorder later.
Against such background, it seems imperative that some service are required for these children, preferably started at an early age. Psychostimulants had been used. (Rapoport, 1978; Taylor, 1985; Werry and Sprague, 1974). It has been demonstrated that it could reduce off-task activities, out of seat behaviour in classroom and restlessness. In fact, the Washington Post 1970 reported 5-10% of a school sample in USA has been taking the drug, and such unskeptical use of medication has created much criticism in the public. Nevertheless, the psychobehavioural effect of psychostimulants is not unique to hyperkinetic children. Similar clinical effect occurred in normal children as well (Rapoport, 1978). Against this short-term efficacy, however, the long-term value of psycho- stimulants in altering the prognosis in hyperactive children has not been established. (Taylor, 1985). In fact, from the available date, there is no difference between the treated and untreated group 5 years after referral. It appears that some conjunctive therapy are necessary in the comprehensive management of these children. Behavioural therapy (Yule, 1984; Gittelman, 1980) and cognitive behavioural therapy (Douglas, 1984) have been proposed. A combination of stimulants and behavioural therapy is regarded as the best treatment, superior to stimulant or behavioural therapy alone (Leek, 1986).
Despite absence of firm evidence from long-term follow up, it is hoped that such timely intervention with a comprehensive package of behavioural and drug treatment will have a positive effect on the child and alter developmental pathway of these children, thus reducing future psychiatric problems.
However, the delivery of behavioural therapy in a busy out-patient setting, with the very limited time and resources, is notoriously difficult. Without a comprehensive analysis of the child's behaviour, a partial or non-contingent reinforcement might happen which could lead to further deterioration(Douglas, 1984). A failure in treatment would cause considerable frustration and demoralisation to the parents, the children and the staff concerned. To overcome these difficulties, a pilot programme, with a relatively intensive therapeutic input, was established in the Ngau Tau Kok Day Hospital.
THE NGAU TAU KOK DAY HOSPITAL
A child unit for hyperkinetic children was planned and established in Ngau Tau Kok Psychiatric Centre in 1985. The structural alteration was completed and officially opened in April 1989. It offers a day hospital setting for the assessment and treatment of children suffering from Hyperkinetic Disorders or its related behavioural problems and offering advice to their parents.
Structurally, it is a purpose-built, fully air-conditioned area of about 2000 sq. ft. The windows are grilled and the elements.
It was staffed with 1 full-time registered nurse, 1 occupational therapist, and a ward assistant. The visiting medical staff and clinical psychologist were recruited from other psychiatric centres and each provided 2 sessions per week services.
The day hospital provided group therapy sessions for children and adolescents. There are two concurrent groups, one conducted in the morning (for children attending pm schools) and one in the afternoon (for children attending am schools). There were 5-6 places for each group and the clientele were matched for age and IQ. Each was a closed group lasted 12 weeks, 3 days per week, and a parent group conducted collaterally on Friday.
METHOD AND PROGRAMME
The admission criteria were:
1) Aged 3 - 16;
2) Diagnosed as Hyperkinetic disorder, Conduct disorder, Behavioural disorder, or a mixture of the above conditions with or without emotional problems; &
3) Children suffering from autism, psychosis, and with IQ less than 50 were excluded.
Cases were recruited from the psychiatric out-patient clinics, child assessment centres, hospitals or other nonclinical settings such as Special Education Section of Education Department, Student guidance officers/teachers, School headmasters on a territory wide basis. Each child was assessed by the multidisciplinary team for suitability of group treatment.
During the intake and subsequent interviews, the child will be under direct observation, and information will be collected from the parents and school teachers with parents' consent.
Structured questionnaires included:
1) Conners Parent Symptom Questionnaire;
2)Werry-Weiss-Peters Activity Rating Scale (WWPARS);
3)Home Situations Questionnaire, were entered by the parents.
Teachers were given:
l) Conners Teacher Rating Scale or the Behaviour Rating Scale (Kendall & Wilcox) &
2) School Situations Questionnaire.
The questionnaires were entered before the commencement of a group, immediately following the completion and half year after the group treatment. The nurse will observe the mother-child interaction for 10 minutes and charted a command-compliance coding.
The treatment programme consisted of 12 weeks of 3 half-day sessions per week of group attendance and one half-day session per week of parent group led by the clinical psychologist.
The children attended the group in a mimicked classroom setting with curriculum of academic lessons, artscraft, group games, physical exercises, "recesses" and opportunities in doing their school homework assignments. They were being observed, their desirable behaviours being reinforced contingently, their misbehaviours recorded and reflected, and if necessary, timeout or punishment would be administered contingently.
The parents attended group running collaterally with the children group. A psycho-educational package involving various aspects of Hyperkinetic disorders, behavioural modification principles and methods of handling behavioural problems in children were discussed. Emphasis were given to foster parent-child relationship. As many of the parents were frustrated or felt incapacitated in looking after their children, their difficulties were shared and their helplessness and loneliness supported. Individual parent sessions were offered on regular intervals to handle any specific family problems that were inappropriate to discuss in the group or in the presence of the children.
Three outings and a home visit were undertaken during the course of group treatment to allow the staff to make a more comprehensive assessment of the child and his family and the parent-child interaction in various situations. The design of the programme also allowed an initial 6 weeks of drug-free period followed by a 6 weeks of trial of methylphenidate. The efficacy and sideeffects of drugs could be closely monitored. On completion of the programme, 3-10 booster individual sessions might be given to some of the children by the nurse or the occupational therapist, to tackle some areas of handicap (motor clumsiness, self-care skills) that might not be adequately handle in the group.
RESULT AND OUTCOME
There had been totally 39 children treated in the programme. The mean of their age was 8.25 years. S.D. 2.15, with a range of 3.08 to 13.92 years. 35 of them were boys. All families belonged to Social Class III to V except 2 of them who came from Social Class II. 2 Children had birth injury and there were one mild grade mentally retarded, one speech delay, one epilepsy and one child suffering from tics within the group. Only 10 children had received methyl-phenidate treatment during some stage of the programme, owing to the resistance from the parents. Only 2 children dropped off prematurely from the programme.
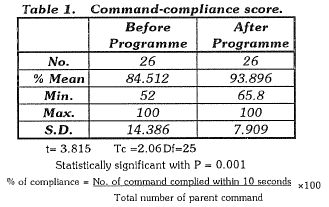
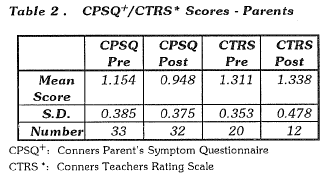
On completion of the treatment, nearly all parents except 4 were found to have improved in the commandcompliance coding (Table 1). The parents also reported that they were more confident in controlling their children. They were more observant of their children's need and behaviour, and they were more positive towards their children and had better mother-child relationship. Most of the parents of children who took methylphenidate were also more satisfied with the children's attention span and activity level. Regarding the Conner's scales, there were also statistically significant improvement reported by the parents in CPSQ score (Table 2).
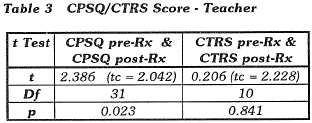
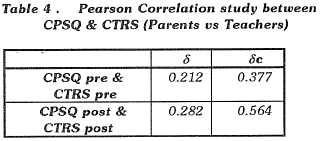
Unfortunately only 20 teachers completed the Conner's Teacher's Rating Scale before treatment, and worse still, only 1/2 of them were able to complete the scale after the treatment programme. There were no significant difference in the children's behaviour before and after the programme as perceived by the teachers (Table 3). There is also poor correlation between the scores rated by the parents and teachers, either before or after the programme (Table 4). The lack of enthusiasm from the school teachers may reflect a communication problem between the centre and the school authority, or a change of teaching staff when treatment programme is completed.
The low drop-out rate from the programme reflected the high enthusiasm and high expectation of parents in the treatment programme. In fact, the parents had to invest a considerable time and effort in order to escort their children to the centre and to attend the parents group themselves. A continual reinforcement of achieving greater skills in child discipline and high morale during the course of treatment were necessary for keeping the programme running. The children had a low rate of absenteeism, which probably also reflected low resistance from the children's part, and many of them expressed they learnt something from the treatment.
CONCLUSION
Shen (1985) in a Beijing school sample, discovered 4.7% of children suffered from Attention Deficit Disorder. Therefore hyper-activity did occur in Chinese children in contrast to the general belief that Chinese are more docile and compliant. Local experience (Luk, 1991) also suggested that the scale of hyperactive problem are comparable to overseas studies. Hence, there would be great demand for managing or to alleviate the behavioural problems in these children. Currently, the majority of these children are either tolerated by their teachers, or handled by the Adjustment Unit of the Special Education Services of the Education Department. Only the more severe or aggressive ones were referred to the psychiatric services and only minimal service could be offered to them by the busy and mundane out-patient setting which were mainly designed for general adult patients.
The Ngau Tau Kok Day Hospital Child Unit is unique amongst the other out-patient and day-patient centres in that it provides a time-limited, intensive, high-quality and expensive service to Hyperkinetic Disordered children exclusively. It offers a close-group therapeutic approach, ecle-ctic in principle, utilising mostly a behavioural modification technique supplemented by group and individual psycho-therapeutic skills; and also drug treatment when necessary.
The low frequency (25%) of children eventually taking drugs echoed the U.K. experience that parents had resistance to drug for behavioural problems in children.
It is not surprising that the restless, inattentive and disruptive behaviour did not improve after the treatment course. Improvement of target ·behaviour should be a long-term and gradual process. The major success in the programme lies in the improved compliance of these child ren to parental commands and the parental satisfaction. It is hoped that with the improved parental confidence, competence and the improved parent-child relationship, it would alter the vicious cycle of negative adult-child interactions and eventually led to an improvement of behaviour. The group treatment programme allow the children an opportunity of reincarnation. They had usually been labelled as bad and problematic for years by various care-takers. Being trained in an acceptive environment with a group with similar problematic children, being accepted, and being rewarded with any small but good behaviour were the opp01tunities that they had often been denied in the past and which they craved and treasured. The parents and caretakers will also get a chance to reconsider their role in relating with their children and readjusting their child handling skills.
The Ngau Tau Kok Day Hospital Child Unit had its own problems. It is a non-educational setting without the valuable teaching support. Hence, the children has to hu rried to or back from school in order to attend the training sessions there in frequent intervals during the training period. They have to spend extra time to complete homework assignment from school. The parents have to make great investment in time and effort to attend the course and great motivation are needed. There have been problems in recruiting suitable cases - probably due to the low publicity of the service, and geographical reasons. It is difficult for some children !iv ing/studying far away to attend the centre. The longterm outcome of improvement is yet uncertain and we suggest that some booster programme are needed to keep the parents and children afresh of the valuable alteration. We expected our experience will stimulate more awareness of the condition and referral to the centre. Also in view of the size of the problem, we believe that with more available services the demand will also increases. We would therefore re-commended that setting up of more service unit on a regional level.
ACKNOWLEDGEMENT
We thank Dr Calais Chan for the statistical advice and Mrs Connie Chau for typing the script.
REFERENCE
Douglas V, (1984) The Psychological Process, Implicated in ADD. In Blooming Dale LM (ed}. Attention Deficit Disorder- Diagnostic, Cognitive and Therapeutic Understanding. New York, Spectrum Publications.
Gittelman R, Abikoff H, Pollack E, Klein D, Katz S & Maltes J, (1980) A controlled Trial of Behaviour Modification and Methyl Phenidate in Hyperactive Children in C Whalen, B Henker (eds}. Hyperactive Children : The Social Ecol ogy of Identification and Treatment. : Academic Press.
ICD-10 (1992) Mental and Behaviour Disorder : Diag nostic Criteria and Diagnostic Guidelines. WHO.
Luk SL, Leung PWL & Lee PLM, (1988) Conners' Teacher Waiting Scale in Chinese Children in Hong Kong. J of Child Psychology & Psychiatry 29 : 2, 165-174.
Luk SL, (1989) A Study on Childhood Hyperactivity : Clinical Observation and A Local Survey. M D Thesis.
Luk SL, et al, (1991) Behaviour Disorder in Preschool Children in Hong Kong. A Two Stage Epidemiological Study. B J Psych. 158 : 213-221.
Rapoport JL, Buchsbaul MS, Zahk T, Weingact, (1978) Dextroamphetamine : Cognitive and Behavioural Effects in Normal Prepubertal Boys. Science 199 : 560-563.
Richman N, Stevenson J & Graham PJ, (1982) Preschool to School : A- Behaviour Study. Academic Press,
Shen YC, Wong YF, Yang XL, (1985) An Epidemiological Investigation of Minimal Brain Dysf unction in Six Elementary Schools in Beijing. J. of Child psycho. & Psychiatry 26 : 777-788.
Taylor E, (1985) Drug Treatment in M Rutter, L Hersov (eds). Child and Adolescent Psychiatry, Modem Approaches. 2nd edition. Oxford Blackwell Scientific Publication.
Werry J & Spraguer, (1974) Methyl-Phenidate in Children : Effect of Dosage. Aust & NZ J of Psychiatry 8 : 9-19.
Yule W, (1984) Behavioural Treatments. The Overactive Child, Clinics in Development Medicine. Heinemann
*C.C.Lee MBBS, MRCP, MRCPsych. Senior Medical Officer, Kwai Chung Hospital.
S.F. Hung MBBS, MRCPsych, DPsych. Consultant Psychiatrist (Child & Adolescent ), Kwai Chung Hospital.
Anna W.Y. Chan MBBS, MRCPsych. Consultant Psychiatrist, Castle Peak Hospital.
* correspondence : Dr.C.C. Lee, Kwai Chung Hospital, Kwai Chung, Hong