J.H.K.C. Psych. (1994) 4, 21-27
ORIGINAL PAPER
SUMMARY
A group of elderly patients suffering from Parkinson’s Disease was studied with the aim of identifying important variables which may affect their outcome and health care needs. Patients were divided into a cognitively impaired group and a non-cognitively impaired group on the basis of their Mini-mental State Examination scores. Our findings indicate that cognitive impairment is not a major predictor for the patients’ daily life adjustment. In contrast, the patients’ behavioural and emotional problems in conjunction with the level of their caretakers’ sense of burden exert the most influence on overall psychosocial adjustment and functional outcome. Recommendations for assessment, identification of early risk signs, and care of elderly patients and their caretakers are suggested.
Keywords: Parkinson's Disease, cognitive impairment, psychological problems, caregiver burden
INTRODUCTION
Parkinson's Disease (PD) is a common neurological problem affecting mainly the elderly. As the population in Hong Kong ages, an increasing number of people is expected to be affected. About 200 patients diagnosed as suffering from PD were being actively treated in the Department of Medicine at Queen Mary Hospital at the time of this study. In addition, there are about 30 new cases per year attending the Movement Disorder Clinic of the department.
Individuals afflicted with PD are often handicapped in multiple aspects. Motor tremors, bradykinesia, and rigidity are the hallmark manifestations of Parkinsonism creating marked inconvenience and adjustment difficulties in everyday life activities. Cognitive impairment is also common although it may vary considerably in quality and severity, ranging from focal deficits to global dementia. The prevalence of dementia in our PD population is 20.6% (Chang, 1993) which is very close to the 24.5% estimated by Brown and Marsden (1984). The Parkinsonic patient also has to endure the onslaught of other discomforts. For example, the antiparkinsonian medication commonly prescribed to such patients, levodopa, was found in some studies to cause acute depression, delusion, hallucination and confusional state (Parkes, 1981). Anticholinergics may induce confusional state and memory disturbances in the elderly patient (De Smet et al, 1982). The chances for developing various other complications are thus heightened, e.g. falls, pneumonia, and fractures. Due to the increased need for dependency; emotional, behavioural, and self-esteem problems are likely to be accentuated. The stresses engendered by the inevitable developmental demands of late life in having to come to terms with old age and one's mortality are also intensified. The functional and adjustment capability of the elderly Parkinsonic patient is thus multi-determined. While the extent of cognitive impairment is conceivably an important factor in influencing functional outcome, other factors including symptom control, side-effects of medications, presence of emotional and behavioural disorders, and nature and quality of the caregiver's skills are equally likely to affect the patient's overall adjustment.
The potentially important inter-dependency between the caregivers' skills, perceived burden, the patients' presenting problems and their functional outcome deserves special attention. Haley et al (1992) noted that compared to other patient populations, family caregivers of demented elderly patients show a comparatively higher level of dissatisfaction with medical care. Their greatest dissatisfactions relate to having insufficient information about the patient's condition and having insufficient referrals for ·supportive services.
While there are some isolated studies in Asia highlighting some of the impo1iant issues in the care of the elderly patient, few systematic studies have been conducted in Hong Kong. In Korea, Kim et al. (1993) studied an elderly demented group of subjects and reported an average of 5.3 mental symptoms in the subjects. Patients with the most mental symptoms have the worst caregiver-patient relationship. In Japan, Kobayashi et al. (1993) drew attention to the developmental process involved in the family caregivers of demented patients, noting that caregiving skills evolve from a beginning phase to an awakening stage where an increasing realisation of the need for measured training and discipline is emphasized.
It is important for mental health workers in Hong Kong to gain a clearer idea of how various issues and factors may or may not be involved in the care of the cognitively impaired or chronically afflicted elderly population. In particular, a clarification of the interrelationships between caregiver burden, the elderly patient's cognitive functioning, daily life adjustment, behavioural and emotional problems is required in our quest for a continual betterment of health care services for the elderly. Outcome in the elderly patient population should necessarily be multi-dimensionally focused, with specific emphasis on the eventual quality of life of the individual concerned. Variables considered impo1iant in rehabilitative concerns include physical well-being, emotional adjustment, cognitive competence, adequacy in daily life adjustment, extent of behavioural and/or mental health problems, as well as the ability to establish satisfactory relationships.
AIMS OF THE STUDY
We are interested in studying a group of elderly patients suffering from Parkinson's Disease, and to outline important variables affecting their outcome and health care needs. The results of our study are expected to have important relevance for the understanding of the needs of other elderly populations given the extensity of the physical, emotional, behavioural and psychological problems in the Parkinsonic patient population. The present study was undertaken with several aims in mind. In particular, several clinically pertinent questions concerning the patients' well-being are posed:
- What is the degree of correlation between various measures of cognitive functioning and functional disability in the elderly Parkinsonic population studied?;
- How are cognitive, psychological, behavioural, emotional and daily life adjustment of the patients and their caregivers' subjective sense of burden related to each other?
- What are the clinical implications of the findings with particular reference to the health care needs of the elderly patients?
METHODS
SUBJECTS
24 subjects were randomly selected from two subgroups of patients followed-up in the Parkinsonic clinic. All subjects recruited had been cognitively screened with the administration of the Chinese translated version of the Mini-mental State Examination (Folstein, 1975), and divided into a cognitively impaired (impaired) and a noncognitively impaired (non-impaired) group. 12 patients were randomly selected from the impaired group with a mini-mental score of less than 20 points (mean= l8. l). Another 12 patients were randomly selected from the non-impaired group with a mean mini-mental score of 30 points.
PROCEDURE
All impaired and non-impaired PD subjects were assessed blind by the first and third author on a number of psychological test measures. In addition, the spouse caregiver in the family was interviewed separately for an assessment of his/her perceived burden and hardships in caring for the sick relative. Various other physical investigations were also conducted and arranged by the second author prior to the psychological assessments.
MEASURES
A cover sheet was designed to record basic background and demographic information on the subjects.
Cognitive and Mental testing
The Kendrick Object Learning Test from the Kendrick Cognitive Tests for the Elderly (Gibson et al, 1975; Kendrick, 1985), the Cantonese version of the Information and the Similarities subtests of the Wechsler Adult Intelligence Scale (Wechsler, 1958) were administered. Emotional symptoms and physical malaise were assessed with a standard symptom checklist (available from the authors). The adequacy of the patients' daily life activities was assessed with the Current Social Adjustment Scale (Lee et al. 1985) adapted from Katz et al. (1963).
Measures administered on the spouse caregivers
When the spouse caregivers were assessed, the following measures were administered:
The Sickness Impact Profile (Bergner et al., 1981), the Barthel ADL Index (Wade and Collin, 1988), a questionnaire on caregiver perceived burden, and a listing of the type and frequency of the behavioural and emotional problems of the patients as manifested in their everyday life. The information gathered provided a comprehensive picture of the patient's daily life activities, physical capability, behavioural and emotional difficulties.
Physical Investigations
For the 12 impaired subjects, complete blood counts, serum T4, VDRL, EEG and Brain CT were performed to exclude other known causes of dementia.
RESULTS
Subject characteristic:
The mean age of the impaired and non-impaired subjects was 64.3 years and 55.2 years respectively (t=2.35, p<0.05). The mean duration since onset of the Parkinson's Disease for the entire subject population was 64.6 months; 95 months (range: 30-211 months) and 68 months (range 42 - 181 months) respectively in the impaired versus the non- impaired subjects (t=2.12, p<0.05). There were no statistically significant differences in the average daily dose of levodopa being prescribed for the two groups of subjects (the mean dose for the impaired versus non- impaired group was 598 mg. and 654 mg. respectively). Of the impaired subjects, 10 were classified as belonging to the akineticrigid-tremor subtype, and 2 were classified as being the akinetic-rigid subtype of Parkinsonism. Of the nonimpaired subjects, 10 were classified as being the akinetic-rigid-tremor subtype while 1 was classified as the akinetic-rigid subtype and the remaining 1 subject classified as being the tremor dominant subtype of Parkinsonism. In addition, 4 impaired subjects and 3 non-impaired subjects had clinical evidence of dyskinesia.
Inter-relationships between different measures of cognitive functioning:
The subjects' mini-mental examination scores were correlated with their respective scores on the Information and Similarities sub-tests of the WAIS, and also with their Kendrick Object Learning Test scores. The subjects' scores on the Similarities subtest and the Kendrick Object Learning Test yielded a significant correlation with their mini-mental state scores (p<0.05). The impaired versus the non-impaired subjects' scores on both tests were also significantly different with the non-impaired subjects scoring higher. The difference in the mean scaled scores obtained by the two groups in the Information subtest of the WAIS is not statistically significant.
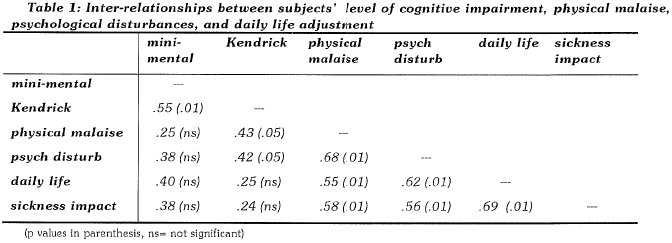
Inter-relationships between subjects' level of cognitive impairment, physical malaise, psychologcal disturbances, and daily life adjustment:
As shown in Table 1 below, there is a moderately significant correlation between the Kendrick Object Learning Test scores and the subjects' complaints of physical malaise and psychological symptoms as observed by caregivers. Measures of psychological and daily life functioning, including indicators of daily life adjustment, impact of sickness, and physical malaise correlated significantly with each other.
Relationship between caregivers' burden, subjects' psychosocial outcome & cognitive impairment:
Caregiver burden was significantly related to the total number of the subjects' manifested behavioural and emotional problems as reported by the caregiver (r=0.66, p<0.01). Caregiver burden correlated significantly with the subjects' Sickness Impact scores (r=0.42, p<0.05), and daily life adjustment (r=0.40, p<0.10). A multiple regression analysis using caregiver burden as the dependent variable and other adjustment and cognitive measures as predictor variables indicated that the largest single predictor of caregiver burden was the total number of the subjects' behavioural and emotional problems (p<0.001). In addition, problems relating to the subjects' anger (p=0.01), hygiene (p<0.05), unaccepting of well-intentioned advice/persuasion (p<0.05), and constant complaining (p<0.05) were also significant in predicting caregivers' sense of burden. The total variance of the caregivers' burden accounted for by all the significant variables in the regression equation amounted to an R square of 0.573. However, caregiver burden was not associated with the level of the subjects' cognitive impairment as measured by any of the cognitive measures.
DISCUSSION
The following discussion will centre around the initial research questions posed.
1 . What is the degree of correlation between the cognitive psychometric testing results, the Mini-mental State Examination scores, and the psychosocial adjustment of the elderly PD population?
It is clear from the results obtained that documented cognitive impairment is neither the only nor the most important variable associated with the elderly PD subjects' functional outcome as measured by their own complaints of physical malaise, daily life activities and adjustment, and independent caregivers' reports on their behavioural and emotional problems. The global indicator of cognitive impairment (as measured by the Mini-Mental State Examination) was not predictive of the various outcome dimensions. The level of functioning in abstract conceptualisation (as measured by the Similarities subtest) and the subjects' long-term memory functioning and retrieval abilities (as measured by the Inormation subtest) were also not associated with any of the outcome measures. However, specific cognitive impairment relating to recall and learning of everyday objects after brief exposures (as measured by the Kendrick Object Learning Test) was found to be associated with complaints of physical malaise and presence of psychological and behavioural disturbances. This finding is understandable in view of the fact that the subjects' daily life adjustment may be more immediately affected by the intactness of their short-term memory and learning abilities rather than their capability in abstract conceptualisation or recollection of events that are long past.
2. How are cognitive, psychological , behavioural, emotional and daily life adjustment of the subjects and their caregivers' reported burden related to each other?
There is a mild intercorrelation between the various indexes measured, indicating a clear inter-dependency between the level of the subjects' cognitive, psychological and daily life adjustment, and caregiver burden. The clinical relevance of the significant interdependency between the variables can be considered from at least two related perspectives. Firstly, any problems in a particular area of the subjects' functioning is likely to implicate and amplify difficulties in other areas of their adjustment. Secondly, intervention with the elderly has therefore necessarily be multi-focused to ensure the best therapeutic results. In fact, the focus would need to go beyond the subjects themselves to a consideration of the actual level of the caregivers' burden.
The PD subjects' manifest psychological and behavioural problems also accounted for a much larger extent of the caregivers' burden compared to that accounted for by the level of their cognitive impairment. There is an average of 4.9 reported psychological problems in our PD subjects. Our findings are similar to the findings of Kim et al. (1993) in Korea indicating an average of 5.3 mental symptoms in their demented subjects. The 5 most commonly reported symptoms noted in our study are slowness, hygiene problems, tiredness/lethargy, uaccepting of well-intentioned advice and persuasion, and pessimism. However, some reported psychological or behavioural problems are more difficult to handle than others. From the caregivers' point of view, these are: the subject being constantly complaining, showing a lot of anger, having hygiene problems, and unaccepting of well intentioned advice and persuasion. The more beavioural and psychological problems the subject manifests, the higher is the level of perceived burden in caring for them.
It should be noted that caregiver burden is not simply an isolated variable. Our results indicate that the higher the perceived caregiver burden, the more likely are subjects to be adjusting poorly in their daily life activities, and the more likely are they to be suffering from multiple symptoms of physical malaise as well. In a cross-sectional study such as ours, we are not able to draw any causative relationship between the above variables. However, the important clinical significance of the heightened inter-dependency between caregiver burden, subjects' behavioural and psychological problems, and the subjects' actual daily life adjustment cannot be underestimated.
It should also be pointed out that none of the demographic and other illness variables collected on the study population were associated with their outcomes. In particular, it is interesting to note that variables including age, sex, age since onset, duration of the illness, subtypes of Parkinson's Disease, daily dosage of levodopa required, CT-scan, EEG, and physical examination findings, were not in any way associated with the subjects' functional and psychosocial outcomes.
3. What are the clinical implications of tl1e findings with particular emphasis on the health care need s of the elderly patients?
The results from our study should obviously be interpreted with caution in view of the small number of subjects studied, and the fact that the subjects may not be representative of the entire elderly population as they were recruited from only one specialist clinic. However, in view of the documented inter-dependency between the subjects' manifest psychological/behavioural problems, their functional outcomes, specific cognitive impairment, and their caregivers' burden; a more significant role for psychological expertise and intervention in helping the elderly PD patients and their caregiver is indicated. Our findings suggest that the functional and psychosocial outcome of Parkinsonic patients is best considered in a multi-factorial model involving cognitive impairments, behavioural and emotional difficulties, symptom control, and caregivers' perceived burden and skills.
Care of the elderly patient involves consideration of not only patient-related factors. Important modulating influences on the patients' outcome and adjustment are likely to come from the family, other caregivers, and the community. An evaluation and treatment plan must go beyond the patient's immediate medical problems to examine the caregiver's needs and the community services available. In fact, Potter (1993) argued that caregiver burden is a better predictor of service use than any other measure of the older person's mental or physical health or functional abilities.
The caregivers' skills and mental health is thus a leitimate area of concern. For example, Baumgarten et al. (1994) noted that caregiver depression, physical symptoms, patients' behavioural problems, and the patients' ultimate institutionalisation are all intimately reated to each other. Caregivers need to be specifically trained to be better equipped with psychological skills in forestalling and dealing with various psychological/behavioural problems in the patients. With more skills and knowledge, the caregivers would presumably develop a better sense of perceived control, effect a more positive relationship with their relativepatients, and thereby helping to ensure the most optimal adjustment possible despite the chronicity of the patients' problems. Perhaps more attention should also be devoted to help caregivers grow and find meanings through their caregiving experiences (Farran et al., 1991) throughout the gradual development of their so called "caregiver career" (Lindgren, 1993). There are also some indications that direct or indirect respite services for the patients and their caregivers may be beneficial (Conlin et al., 1992; Grasse! et al. 1993; Hardy et al. 1993). Within such service framework, caregivers are afforded temporary relief from their burden by having days off, as well as having periodic counselling sessions and participation in self-help groups.
CONCLUSION
Despite their well documented cognitive and physical impairment, the ultimate psychosocial and adjustment outcome of PD patients seems to be heavily dependent on concurrent psychological and behavioural symptoms, as well as their relationship with their caregivers as measured by caregiver burden. Health care workers need to be particularly aware of certain high risk signs in the patients which may hamper the patient-caregiver relationship as well as complicating the patients' ultimate daily life adjustment. The high risk signs highlighted in this study are: significant impairment in short-term memory and learning abilities, the patient being constantly complaining, showing a lot of anger, having hygiene problems, and unaccepting of well intentioned advice and persuasion. In addition, the more behavioural and psychological problems the patient manifests, the more significant would be the negative effect.
Further studies, particularly those with a longitudinal design, are called for to look into the "career of the caregiver process", and in highlighting the vital interdependency between the patients' problems and the caregivers' sense of burden and well-being.
REFERENCES
Baumgarten, M., Hanley, J.A , Infante-Rivard, C., Battista, R N. , Becker, R , Gauthier, S. (1994). Health of family members caring for elderly persons with dementia: A longitudinal study. Ann. Internal Medicine 120(2), 126- 132.
Bergner, M., Bobbitt, R A , Carter, W.B., Gibson, B.S. (1981) The Sickness lmpack Profile: development and final revision of a health status measure. Medical Care, 19, 789-805.
Brodaty, H., McGilchrist, C,, Harris, L., Peters, KE.(1993). Time until institutionalization and death in patients with dementia. Arch. Neurology, 50(6), 643- 650.
Brown, R G., Marsden, C.D. (1984). How common is dementia in Parkinson's Disease? The Lancet, Dec. 1, 1262-1265.
Chang, C.M. (1993) Parkinson's disease in Hong Kong - a study of 234 Chinese patients in a movement disorders clinic. J.H.K.Medical Association, 45(1), 19-23.
Conlin, M.M., Caranasos, G.J., Davidson, R A (1992) Reduction of caregiver stress by respite care: a pilot study. South Medical Journal, 85(11), 1096-1100.
De Smet, Y., Ruberg, M., Serdaru, M. , Dubois, B., Lhermitte, F., Agid, Y. (1982). Confusion dementia and anticholingerics in Parkinson's disease. J. Neurol. Neurosurg. Psychiatry, 45, 1161-1164.
Farran, C.J., Keane-Hagerty, E. , Salloway, S., Kupferer, S., Wilken, C.S. (1991) Finding meaning: an alternative paradigm for Alzheimer's disease family caregivers. Gerontologist, 31(4), 483-489.
Folstein, M.F., Flostein, S.E., McHugh, P.R. (1975) Minimental State: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189-198.
Gibson, A.J., Kendrick, D.C. (1979) The Kendrick battery for the detection of dementia in the elderly. The NFER Publishing Company Ltd.
Graftstrom, M., Norberg, A., Hagberg, B. (1993) Relationships between demented elderly people and their families: a follow-up study of caregivers who had previously reported abuse when caring for their spouses and parents. J. Adv. Nursing, 18(11), 1747-1757.
Grasse!, E., Orbens, H., Senf , T. (1993) A concept for relieving family caregivers - the Dreycedern Project: a prototype facility for demented patients. Rehabilitation Stuttgart, 32(2), 134-138.
Haley, W.E., Clair, J.M. , Saulsberry, K (1992) Family caregiver satisfaction with medical care of their demented relatives. Gerontologist, 32(2), 219-226.
Hardy, V.L., Riffle, K L. (1993) Support for caregivers of dependent elderly. Geriatric Nursing, 14(3), 161- 164.
Katz, M.M. , Lyerly, S.B. (1963) Methods for measuring adjustment and social behavior in the community p I. rationale, description, discriminative validity scale development. Psychological Reports, 13, 503-535.
Kendrick, D.C. (1985) Kendrick cognitive tests for the elderly. The NFER-Nelson Publishing Company.
Kim, E. , Takeo, K , l{imura, K (1993) The study of senile symptoms and home care on the elderly living in Korea. Nihon-Kango-Kagakkaishi, 13(2), 37-44.
Eobayashi, S., Masaki, H. , Noguchi, M. (1993) Developmental process: family caregivers of demented Japanese. J.Gerontological Nursing, 19(10), pp. 7-12.
Lee, P.W.H., Ho, E.S.Y. , Tsang, A.KT., Cheng, J.C.Y., Leung, P.C., Cheng, Y.H., Lieh-Mak, F. (1985) Psychosocial adjustment of victims of occupational hand injuries. Social Sciences and Medicine, 20(5), 493-497.
Lindgren, C.L. (1993) The caregiver career. Image Journal of Nursing Science, 25(3), 214-219.
Mangone, C.A., Sanguinetti, R.M., Baumann, P.D. , Gonzalez, R.C., Pereyra, S., Bozzola, F.G., Gorelick, P.B., Sica, R.D. (1993) Influence of feelings of burden on the caregiver's perception of the patient's functional status. Dementia, 4(5), 287-293.
Parkes, J.D. (1981) Adverse effects of anti-parkinsonian drugs. Drugs, 21, 341-353.
Potter, J.F. (1993) Comprehensive geriatric assessment in the outpatient setting: population characteristics and factors influencing outcome. Exp. Gerontology, 28(4-5), 447- 457.
Sistler, A.B., Blanchard-Field, F. (1993) Being in control: a note on differences between caregiving and noncaregiving spouses. J. Psychology, 127(5), 537-542.
Wade, D.T. , Collin, C. (1988) The Barthel ADL index; a standard measure of physical disability? International Disability Studies, 10, 64-67.
Wechler, D. (1958) The measurement and appraisal of adult intelligence, 4th ed. Baltimore: Williams & Wilkins.
*Peter W.H.Lee MSocSc (ClinPsy), PhD Sen ior Lecturer in clinical health psycholog y, Depa rtment of Psychiatry, The Un iversity of Hong Kong
Paul Chang Chee-My,MBBS, FRCP Chief of Service, Depa rtment of Medicine, Ruttonjee Hospital
Amy S.M.Fung,MSocSc(ClinPsy) Clinical Psychologist, Queen Ma ry Hospital
Patrick W.L.Leung MSocSc(ClinPsy), PhD Lectu rer in clinical psychology, Depa rtment of Psychology, The Chinese University of Hong Kong
* Correspondence: Dr. Peter Lee, Senior Lecturer, Depa1iment of Psychiatry, Queen Mary Hospital, Pokfulam Road, Hong Kong.