Hong Kong Journal of Psychiatry (1995) 5, 25-29
SPECIAL TOPIC: FORENSIC PSYCHIATRY
Summary
A sample of 134 consecutively admitted patients for schizophrenia or schizophrenic disorders was assessed by sociodemographic information, the BPRS, the 12-item Symptom Rating Scale, the BEP and the MMPI. The MOAS was administered to evaluate the dangerous behaviour during the first 15 days of hospitalization. Compared with the control group, 41 patients with dangerous behaviour had longer duration and higher frequency of hospitalizations, more previous history of violent behaviour, higher scores on thought-disturbance, hostile-suspiciousness and activation of BPRS, more abnormalities of BEP, and higher scores on L, F, K, Pd, Ma of MMPI. The fully completed data of 82 patients were analyzed by logistic regression and a predicting model was developed. Six variables were identified, namely: hostile-suspiciousness and activation of BPRS, abnormality of BEP, F and Pd of MMPI, auditory hallucination of command. The model was validated with sensitivity of 86.7% and specificity of 92.3%.
Keywords: schizophrenia, Chinese, dangerousness, variables, logistic regression
INTRODUCTION
Mental health acts were issued in many countries, in which the legal basis for compulsory admission and detention of psychiatric patients were strictly provided. It is stated that the patients must be a danger to themselves or others because of mental disorders, and when the danger is removed, the patient should be discharged. Therefore, workers in mental health and forensic fields are facing a difficult problem, how to judge or predict the dangerousness of a psychiatric patient.
Towards the end of the 1970's, the prediction of dangerousness stepped into a new era called "the second generation of prediction." With the advances of statistical methods and instruments, research outcomes become more and more standardised and the accuracy of prediction has improved.
In the People's Republic of China, most of the researches conducted so far could only be part of the first generation of prediction, in which data were collected and the possible predictors descriptively analyzed. This study aims to probe into the feasibility of predicting dangerousness amongst Chinese psychiatric inpatients, and thus to find out the factors associated with dangerousness.
METHODOLOGY
SUBJECTS
The sample was selected from two wards in Shanghai Mental Health Centre, one for male and one for female. The subjects were those who were diagnosed as schizophrenia or schizophrenic disorders, according to Chinese Classification and Diagnostic Criteria of Mental Disorders, 2nd Edition, who were consecutively admitted to these two wards between Jan. 1to Nov. 31, 1991. During the first 15 days of hospitalization, a Modified Overt Aggression Scale (MOAS) (Kay, 1988) was used to assess the dangerous behaviour occurred in each patient. Those patients, who got the weighted total scores of more than 4, were selected into "violent" group, while the rest entered the "nonviolent" control group.
PROCEDURES
Within the first seven days of hospitalization, the newly admitted patients were assessed by sociodemographic information (self-designed) and the Brief Psychiatric Rating Scale (BPRS). During the first fifteen days of hospitalization, each patient was assessed by MOAS according to the nursing records. In the first month of hospitalization, each patient was assessed by the "12-item Symptom Rating Scale," which was devised on the basis of PSE and SAPS, and each item consisted of three ratings. A Brain Evoked Potentials (BEP) and the Minnesota Multiphasic Personality Inventory (MMPI) were administered before the patients were discharged. All the significant testings and logistic regression were made on the software of Biomedical Computer Programmes.
RESULTS
Among the sample of 134 (74 of male and 60 of female), 82 patients finished all the examinations designed (46 of male and 36 of female). There was no group difference on sex (U=0.02, p>0.05). The other 52 patients (38.8% of the sample) failed to completed the BEP and/or the MMPI because of incorporation or low education. So single factor analysis was based on the actually finished data on each index, while multiple analysis was conducted on the fully completed data of 82 patients. All patients completed the sociodemographic information, the BPRS, and the 12- Item Symptom Rating Scale. According to the result of MOAS, 41 entered the violent group, while 93 formed the control group. Of the 82 patients who completed the BEP and MMPI, 30 were in the violent group and 52 in control group. There was no significant difference on the group proportion (U=0.91, p>0.05).
SOCIODEMOGRAP HIC INFORMATION
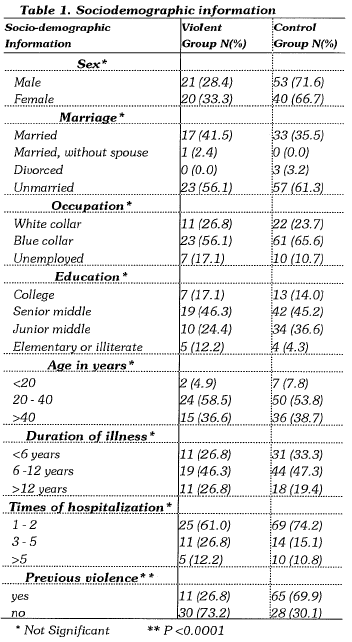
There was no group difference on sex, age, marriage, occupation, education, duration of illness and frequency of hospitalization. The history of previous violence was more prevalent in the violent group (Table 1).
BPRS SUBSCALE SCORES
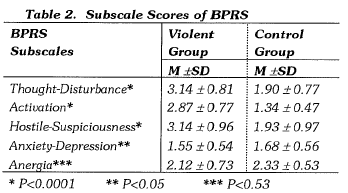
The violent group scored higher on the three subscales of BPRS, namely: Though-Disturbance, Activation and Hostile-Suspiciousness. However there was no significant difference reached on Anxiety-Depression and Anergia (Table 2).
BRAIN EVOKED POTENTIALS (BEP)
The results were scored 1 to 3 where 1 indicated normal, 2 indicated mildly abnormal and 3 indicated severely abnormal. The average score of the violent group was 1.27±0.74, while the control group was 0.53±0.61. The result suggested that the violent group had more frequent abno1malities of BEP, and the abnormalities tended to be severe.
MENTAL STATE
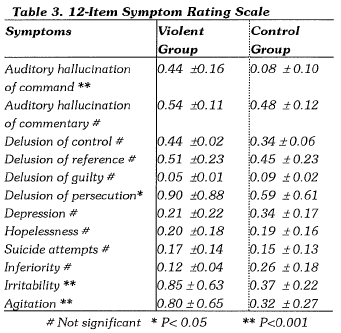
The violent group got significantly higher scores on auditory hallucination of command, delusion of persecution, irritability and agitation of the 12-Item Symptom Rating Scale. There was no group difference on the other symptoms (Table 3).
MINNESOTA MULTIPHASIC PERSONALITY INVENTORY (MMPI)
The violent group got higher scores on L, F, K, Pd, and Ma. There was no significant difference on the other subscales (Table 4).
STATISTICAL MODEL
In order to establish the predicting relationship between each possible factor and the dangerous behaviour, data of the 82 fully completed subjects were processed by logistic regression, in which 41 factors were used as independent va1iables and the outcome of MOAS as dependent variable. Six variables identified were: Activation and Hostile-suspiciousness of BPRS, Auditory hallucination of command, abnormality of BEP, F and Pd of MMPI (Table 5).
These six selected factors were then computed and the odds ratios obtained for each patient. The patients were first ranked by odds rations with the assumption that ilie higher odds ratios would be found among the 30 violent patients. The sample of 82 patients were then divided into two sets. Patients ranked 1 to 30 were know to be violent, and patients ranked 31 to 82 were know to be nonviolent. The usefulness of the odds ratios in classifying violent and nonviolent patients was evaluated. The sensitivity was 86.7% and the specificity 92.3%. The total accuracy was 90.2%. The results indicated the model got a high level of accuracy in prediction.
DISCUSSION
Up to now, there was no generally accepted definition of dangerousness. In literature, dangerousness was always equivalent for terms such as violence, assault, aggression, than nonnal people, while schizophrenia was the most dangerous among all the psychiatric disorders. The present study showed that the incidence of dangerous behaviour in schizophrenia patients was 30.6%. However, physical assault was not so prevalent. Only 13 patients were involved in physical assault, about 9.7% of the sample. And they all scored low on MOAS. Only one patient had a mild injury which did not need any special management. The finding supported the other reports that seriously violent events seldom occurred in hospitals (Davis, 1991).
Many studies tried to find the predicting factors from vital statistics and hospitalization data (Palmstiema & Wisted, 1989, Convit et al, 1989, McNiel et al, 1988). In the past, it was generally believed that these factors were related to the dangerous behaviour of inpatients who were male, youthfulness, of low education, low social-economic sihtation, with deviant family environment in childhood, history of alcoholics and substance abuse. The present sh1dy indicated that except for the history of previous violent behaviour, the other factors mentioned above failed to reach statistical significance. Many papers reported that previous violent behaviour had a positive correlation with subsequent dang-erous behaviour of hospitalization. Therefore, Blomhoff (1991) pointed out that the history of previous violence might be the best predictor of dangerousness of inpatients. Recently, the view about the relationship between sex and dangerous behaviour changed a lot. In this study, we found that female inpatients had a higher rate of incidence than male inpatients (33% versus 38%) which might result from the fact that more female inpatients involved in verbal assault. However, the difference did not achieve statistical significance.
This study demonstrated that the subscale score of BPRS could be used as predictors of dangerous behaviour in the early phase of hospitalization. The violent patients scored higher on the following subscales: thought--disturbance, activation and hostile-suspiciousness. The result suggested the newly admitted patients tended to be excited, restless, hostile and initable, and this supported the findings of Tanke (1985), Palmstiema & Wisted (1989) and Lowenstein (1990).
The symptoms of auditory hallucination of command, delusion of persecution, irritability and agitation of schizophrenia were significantly related to the dangerous behaviour. It was pointed out in previous studies that patients with hallucination and delusion and schizophrenia of the paranoid type were more frequently dangerous at the beginning of hospitalization, while depressive and negative symptoms were inversely related to the dangerous behaviour.
This study showed that the violent group had more abnormalities of BEP which tended to be severe and suggested that the BEP could be a reliable predictor. Fishbein and associates (1989) reported that violent patients not only demonstrated decreased a activities and increased 8 activities in frontal lobe, but also the abno1malities of Brain Stem Auditory Evoked Response (BAER). However, as mentioned by Hemich (1989), by the time of examination of BEP, these patients had often received heavy doses of medications for a certain period of treatment and even special treatment such as electroconvulsive therapy. So it is too early to ascertain whether the BEP outcome was primary or secondary, and fu1iher well-designed studies should be conducted.
The MMPI could be a useful instiument for prediction. The violent patients scored higher on F, K, L, Ma and Pd subscales of MMPI. In particular, F and Pd had strong prediction of becoming assaultive. The result also indicated the characteristics of dangerous patients, viz.: resent, agitation, intolerance, immature and self-centred, etc. which suppo1ied the study of Mungas et al (1989).
Some factors were combined to affect the outcome. In this study, duration-times of hospitalization were analyzed in coordinance. It appeared that the violent group was significantly different from the control group (p<0.05) and the results suggested that patient with longer period of hospitalization and more frequent admissions were at a higher risk of dangerous behaviour. Palmstienna (1991) reported 80% of violent events were committed by 49% of the inpatients. Pearson and associates (1986) found that among the 149 violent events, 56 were committed by 8 schizophrenic inpatients, and these patients had long duration of hospitalization with poor responses to treatment. So those chronic patients with frequent admissions to hospital because of violent behaviour could be the at-1isk group for dangerousness and accurate prediction could prevent dangerous behaviour from happening. Together with a history of previous violence, these could be powerful predictors in distinguishing violent from nonviolent patients. Nevertheless, fu1iher sh1dies were still required.
Although the prediction model achieved a high level of accuracy in this study, there was not enough time to complete all the prospective tests of clinical value. Sometimes examinations by the BEP and the MMPI were hard to perform and therefore the generalizability of the present findings might be limited. Furthermore, in this pilot study, the sample size was not large enough to explore the various social factors such as the family environment, the interpersonal relations11ips, the environment of the ward and the voluntary versus involuntary admission issue, etc.
More comprehensive and accurate predicting methods would therefore be justified in future studies.
CONCLUSION
The issue of how to identify the dangerousness of psychiatric patients was eminently needed as it could benefit the medical, social and legal services. Based on the fact that some psychiatric patients did continuously commit dangerous acts, some prediction should be possible. This present study suggested that schizophrenics did have high incidents of dangerous behaviour within the first few weeks of hospitalization, and some factors could predict such behaviour. These were past violent behaviour, certain subscale scores of the BPRS, specific psychiatric symptoms, abnormalities of the BEP and the MMPI, and the combined factor of duration and time. The logistic regression model used in this study showed a high odds ratio winch should be tested further in future studies.
REFERENCES
Blomhoff S., Seim S. and Friis S. (1990) Can prediction of violence among psychiatric inpatients be improved? Hospital and Community Psychiatry 41: 771-775.
Convit A (1988) Predicting assaultiveness in psychiatric inpatients. Hospital and Community Psychiatry 39: 429-434.
Davis S. (1991) Violence by psychiatric inpatients. Hospital and Community Psychiatry 42: 585-589.
Fisbein D.H. (1989) EGG and brainstem auditory evoked response potentials in adult male drug abusers with self-reported histories of aggressive behaviour. Biological Psychiatry 26: 595-611.
Hellerstein D. (1987) The clinical significance of command hallucinations. American Journal of Psychiatry 144: 219-221.
Hemrichs R.W. (1989) Frontal cerebral lesions and violent incidents in chronic neuro-psychiatric patients. Biological Psychiatry 25: 174-178.
James D.V. (1990) An increase in violence on an acute psychiatric ward. British Journal of Psychiatry 156: 846-852.
Kay S.R., Wolkenfeld F. and Murrill L.M. (1988) Profiles of aggression among psychiatric patients. Journal of Nervous Mental Disease 176: 539-557.
Krakowski M., Volavka J. and Brizer D. (1986) Psychopathology and violence. Comprehensive Psychiatry 27: 131-148.
Kruesi M.J .P. (1990) Cerebrospinal fluid monoamine metabolites, aggression and impulsivity in disruptive behavior disorders of children and adolescents. Archives of General Psychiatry 47: 419-426.
Lidberg L. (1985) Homicide, suicide and cerebrospinal fluid 5- HIAA. Acta Psychiatrica Scandinavia 71: 230-236.
Lowenstein M. (1990) The relationship between admission symptoms and hospital assaults. Hospital and Community Psychiatry 41: 311-313.
McNiel D.E. and Binder R.L. (1991) Clinical assessment of the risk of violence among psychiatric inpatients. American Journal of Psychiatry 148: 1317-1321.
McNiel D.E., Binder R.L. and Greenfield T.K. (1988) Predictors of violence in civilly committed acute psychiatric patients. American Journal of Psychiatry 145: 965-970.
Mungas D. (1989) Psychometric correlates of episodic violent behavior. British Journal of Psychiatry 152:180-187.
Palmstiema T. (1991) The relationship of crowding and aggressive behavior on a psychiatric intensive care unit. Hospital and Community Psychiatry 42:1237-1240.
Palmstiema T. and Wisted B. (1989) Evaluation of the Brief Psychiatric Rating Scale in relation to aggression behavior by acute involuntarily admitted patients. Acta Psychiatrica Scandinavia 79: 313-316.
Pearson M. (1986) A study of violent behavior among inpatients in a psychiatric hospital. British Journal of Psychiatry 149: 416-1419.
Tanke E.D. and Yesavage J.A. (1985) Characteristics of assaultive patients who do and do not have visible cues of potential violence. American Journal of Psychiatry 142: 1409-1413.
*Xie Bin MD Psychiatrist, Shanghai Mental Health Centre
Zheung Zhan Bei MD Psychiatrist, Shanghai Mental Health Centre
* Correspondence: Shanghai Mental Healili Centre, 600, Wan Ping Nan Road, 200030, Shanghai, People's Republic of China