Hong Kong Journal of Psychiatry (1995) 5, 43-49
ORIGINAL ARTICLE<
Summary
As health resources are limited, health services have to be prioritised. In actual practice, such prioritisation is frequently determined by the perspective of the policy makers. A clinician’s perspective can be quite different from that of a public health planner. The situation in Hong Kong for development of psychiatric services is discussed in the light of these two angles.
Keywords: psychiatric service, priorities, epidemiology, public health, Hong Kong
INTRODUCTION
It is quite difficult to determine priorities in clinical services as practically all of them are concerned with morbidity and/or mortality. Since the history of psychiatry is relatively short in Hong Kong, there are many important areas within the psychiatric service which need further development. However, even for the most wealthy countries, there are only limited health resources for allocation. One must therefore act objectively, responsibly and selectively in determining priorities in health care planning, with adequate practical and theoretical support.
In real life, however, the standpoint and even prejudices of the evaluator often affects his or her choices, not to mention personal likings and prejudices. The perspectives for priority setting of a clinician and that of a public health administrator can be quite different and they are discussed below.
PRIORITIES FROM THE CLINICIAN'S PERSPECTIVE
For a clinician, priority of service is often guided by the prevalent disease pattern; and epidemiological studies become paramount. Despite the scarcity of data in mental disorders in Hong Kong, there are still some statistics available at different levels:
LEVEL 1. PATTERN OF MENTAL DISORDER SEEN IN PSYCHIATRIC PRACTICE
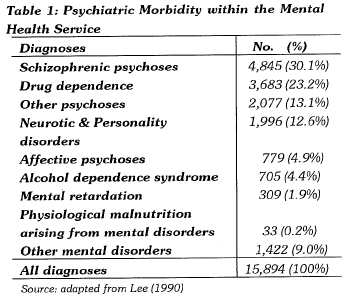
The basic information could be obtained from the official statistics provided by the Hong Kong Government. For example, in the 1988/89 report of the Director of Medical & Health Department (Lee, 1990), the figures for in-patients are listed in Table 1.
The table suggested that 'psychotic disorders' formed the most common problem, to be followed by 'drug dependence', 'neurotic' and 'personality' disorders.
There are a number of methodological problems in this presentation. The figures only reflected those who were hospitalised, and had omitted those who attended outpatient clinics. There do exist some unpublished reports containing detailed statistics about psychiatric services including out-patient service, and they should also form part of the reference material in considering priorities.
Besides, the item on drug dependence cannot be truely representative of the situation in Hong Kong, as the majority of them were treated by specific drug detoxification centres managed by a non-government organisation.
Furthermore, there are also much controversies in Hong Kong concerning whether 'mental retardation' per se should be considered a psychiatric disorder. If it were included, then the majority of mentally retarded persons in the community would be missed from the table.
Lastly, the above pattern is markedly different from that in private psychiatric practices (Mak & Wong, 1988) which comprises a large proportion of neurotic disorders. Henceforth, the government statistics may in a sense be misleading in representing the disease pattern in Hong Kong.
LEVEL 2. PATTERN OF MENTAL DISORDER
SEEN IN PRIMARY CARE
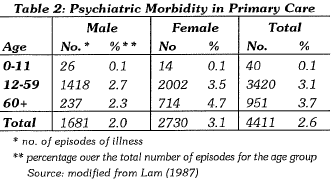
Psychiatry is a specialty within Medicine, and psychiatrists often see patients who are most disabled. In fact, many general practitioners are fairly competent in treating mental illness, especially the minor psychiatric disorders (Shepherd et al, 1981) though it is doubtful whether primary care doctors in Hong Kong are enthusiastic in treating these patients. Unfortunately, there has not been any formal comprehensive study in Hong Kong in this area for various reasons (lack of a formal family medicine service, freedom to doctor shopping, poor medical recording at primary care out-patient clinics, etc.). A multi-practice survey in 1985 (Lam, 1987) reviewed 2% of male patients and 3.1% of female patients (Table 2) attending general medical practitioners complaining of 'mental problems'. The exact type of psychiatric morbidity of this averaged 3.1% of the total patient population was unclear. A more recent survey has been conducted by the Hong Kong College of General Practitioners (Chan, K.C., personal communications) and the results can be useful. Information from the United Kingdom can also be of help, since medical practice in Hong Kong follows closely that of the British system. The authoritative study by Casey (1990) in Ireland is also worthy of reference. In her study of patients attending general practice, 'neuroses' of various types dominate the scene. There was quite a high percentage of 'psychiatric associated conditions' such as 'psycho-somatic conditions' and 'organic illness with psychiatric overlay'.
LEVEL 3. PATTERN OF PSYCHIATRIC MORBID ITY IN THE COMMUNITY
In the past, there is little data about psychiatric morbidity in the community, and service provisions are based on data from patients at the clinical level. In 1979, there was a community survey which reported a 7.8% males and 15.0% females of the Hong Kong population who scored above the critical distress scale for psychological distress (Miller, 1979). Again, there was no breakdown of the morbidity pattern.
Recently, a report was released (Chen et al, 1993) which provided basic information about the psychiatric morbidity of a populated region in Hong Kong (see Table 3). Though this research had its limitations (e.g. it had not included patients residing in that community but hospitalised outside the region), it did give an indication of the current psychiatric problems in Hong Kong.
Furthermore, it should be noted that tobacco dependence per se, though a health hazard, is practically speaking not treated as a psychiatric disorder in Hong Kong. Therefore, the predominant disease pattern found in the study was dominated by 'neurotic disorders' (items 2, 4, 5 & 9 in the Table) and 'alcohol related psychiatric disorders'. This pattern was relatively consistent with the findings by Casey (1990) mentioned above.
With all the data discussed above and with the historical planning of services by psychiatrists without proper training in health planning or public health, it is therefore understandable why clinicians do propose that priorities be given to treatment of disease entities through the continuous establishment of more psychiatric hospitals and clinics, and the emphasis on the provision and training of more qualified professionals at the tertiary care level.
PRIORITIES FROM THE PUBLIC HEALTH PLANNER'S PERSPECTIVE
From the public health planner's point of view, the most important mental health problems are not disease entities, but health-related psycho-social, economic and sometimes political problems (Lawson, 1991). Not that epidemiological findings of diagnostic categories are not important, but the most significant determinants may be the impact or effects of the particular mental problem on the society, the imminence or urgency of time in solving the problem, the availability of financial and human resources to tackle the problem, the cost-benefits of such service provisions, and the acceptance by the public, etc.
Using some of these criteria as an exercise, the author attempts to propose another perspective in setting priorities for the development of psychiatric services in Hong Kong; and each area is breifly presented below.
1. CHILDHOOD PSYCHIATRIC DISORDERS
There is yet no figure of the overall prevalence of childhood psychiatric disorders in Hong Kong and the information from clinics (Chen, 1986) could not represent the community needs. Other countries report a 5 to 10% prevalence rate (Graham, 1979). What matters most is that these patients usually have a normal life span and thus a high index of 'QALY' or quality adjusted life-years (Williams, 1985). Though whether this QALY concept can be applied accurately to psychiatry (Oyebode, 1994), it is obvious that if these disorders are left untreated, they may cause life-long handicaps, and the costs of such long-term management will be astronomical. In particular, treatable childhood developmental disorders like autism (Hung, 1993) or hyperkinetic disorder (Mak, 1993) should merit serious attention when the hardship to the carers and the shortfalls in the community are seriously considered.
2. REHABILITATION OF CHRONIC PSYCHOTIC DISORDERS
In fact, caring for this category of patients (suffering mainly from schizophrenic, affective and organic psychosis) in institutions has been extremely costly to many governments, and also repugnant to the public in developed countries. Developments in community rehabilitation se1vices (Mak, 1991) are essential for their successful reintegration into the Hong Kong society, and the Hospital Auth01ity has already shown signs of development in this area by the approval of specialised multi-disciplinary community psychiatric teams in Hong Kong. If left uncared for, many would become homeless (Street, 1986) and may end up in street comers or in prisons. Innovative projects in the area on reintegration into the community (Chamberlain, 1989) had been quite rewarding, not only because they are cost-beneficial but also they bring satisfaction to the patients and their relatives (Mak & Gow, 1992). A governmental report estimated that there are currently more than 20,000 chronic mental patients requi1ing rehabilitation services (Hong Kong Government, 1991), though experts in the service field estimated a much higher number.
3. PSYCHO-GERIATRIC DISORDERS
As the population of Hong Kong ages, there is an ever-increasing morbidity among the aged. The traditional Chinese filial culture of caring for the parents is disappearing, and is further aggravated by many young healthy persons emigrating abroad. Local research in this area of lack of care is scarce, except perhaps the study by Pan (1989) on parasuicide in the elderly. Among the various categories of mental disorders, functional disorders (anxiety, depression and other neuroses) is most prevalent, and they cause a lot of sufferings. Senile dementia, though not as common as in developed countries (Lo, 1982), is also significant because of its disabling effects on the patients and their carers. Though the gain in expected life-years cannot be too large for these elderly patients, the quality of life' at this final stage of life deserved undeniable moral attention. Again in recent years, the Hospital Autho1ity has set up a few psychogeriatric teams in different regions of Hong Kong.
4. SUICIDE AND PARASUICIDE
According to Lo and Leung (1985), the annual suicide rate per 100,000 population aged over 15 is 18.1. It has been a significant cause of death especially among the older age-groups (Pan, 1989) and among schizophrenics (Cheng et al, 1989) in Hong Kong. In recent years, the issue of childhood and adolescent suicide (Chan, 1993) has caught much publicity in the mass media. The number of 'life-years' lost by suicide is considerable, especially when the commonest method by jumping from high-rise buildings is often fatal, if not paralysing.
The prevalence of parasuicide is rather difficult to obtain, as the practice of reporting is quite varied (Leung and Lo, 1984). Obviously, parasuicide should be much commoner than suicides and is estimated to be eight to ten times the rate of suicide (Kaplan & Sadock, 1988), and this is the group which needs professional help. In fact, some suicide attempters would not repeat the act if properly managed and can be considered 'cured'. At present, there is some information about the high risk factors (Gelder et al, 1984). Hence, psychiatric aftercare for all at-risk parasuicide patients can in the long run substantially lower the loss of manpower and productivity to the society.
5. PSYCHIATRIC DISORDERS RELATED TO ALCOHOL ABUSE
The issue of alcoholic dependence is an obvious finding in the community survey (Chen et al, 1993), but dependence of soft and hard drugs is more notorious in Hong Kong which, as a cosmopolitan city, has attracted international attention. In certain sense, psychiatric complications arising from alcoholism in Hong Kong is not as serious as in other developed countries (Leung, 1991), perhaps related to some enzymatic protection of a high percentage of the Oriental population (Ewing & Rouse, 1976). However, the psycho-social consequences can be very alarming (Shum, 1981; Singer, 1972), as the sale of which is very profitable; and the news of students dying from substance abuse always induce public alarm. So far, special psychiatric rehabilitation detoxification centre for alcoholism in Hong Kong is non-existing, and relapse or recidivism is high. To curtail such a political, socioeconomic and legal problem, a higher priority than the present should be given to this area of service.
It must be added here that service for drug dependence is not unimportant, but the management of hard drug users is currently outside the realm of public psychiatric service, though the Hospital Authority plans to have a special unit for soft drug dependence patients. It may also be objectional to some that the more common neurotic and personality disorders found in the hospital statistics (Lee, 1990) and the community survey (Chen et al, 1993) are not given top p1iority attention. This is deliberate because from a public healthpoint of view, the hardship from such disorders are not uniformly serious, and many can be well looked after by p1imary care providers without in--depth psychiatric training. Mann et al (Mann et al, 1981) found that 50% who attended general practitioners recovered within a year. Those serious enough to merit specialised psychiatric care are actually not too many. In fact, many often recover spontaneously without treatinent, as Tennant et al (1981) found that 50% of community identified cases recover within three months. Definitely, some of these patients could pose serious suicidal 1isks, but this issue had already been highlighted above.
The above description is just an exemplary and admittedly somewhat subjective discussion about priority setting and there are other detem1inants (as mentioned above) that must be considered; and further refinement and improvement are needed before they are being implemented. In certain sense, the urgency of service development may fluctuate with time, and other new categ01ies of needs (e.g. psychiatric care of accident victims) may be added in the future when the demands become phenomenal.
CONCLUSION
Mental health problems do create significant public health issues in Hong Kong. Some people may probably not agree to the use of statistics in prioritising services, while others may object to the use of non-clinical psychosocial detem1inants in psychiatric service planning. Quite often, service planners may not be sufficiently knowledgeable about psychiatric disorders and their significance, and many experienced psychiatrists are not aware of the public health aspect either. On occasions, these two professional groups do not agree with each other in the setting of priorities, leading to prolonged discussions and delayed implementations. As a result, the patient population suffers. Hopefully, this paper can stimulate both concerned parties to have more interests in the epidemiology of psychiatric morbidity as well as the principles of public health, so that clinicians and administrators can come together to design the most costeffective and cost-beneficial service development for Hong Kong.
One final note of caution should be mentioned - that public health principles are best at macro-allocation decisions. When micro-allocations are needed, e.g. in distrubtion of resources to different sectors, in the training of various staff and the development of different treatment programmes, etc., unique features in each situation (e.g. the age group distribution in the area, the socio-economic background, etc.) must also be considered.
REFERENCES
Casey, P.R. (1990) A guide to psychiatry in primary care.
Wrightson Biomedical Pub. Ltd. Petersfield, U.K. Chamberlain, M.A. (1989) What is rehabilitation? British
Journal of Hospital Medicine, 41, 311. Editorial.
Chan, T.S. (1993) Suicide among children and adolescents in Hong Kong. Journal of the Hong Kong College of Psychiatrists, 3, 19-27.
Chen, C.N., Wong, J., Lee, N., Chan-Ho, M.W., Lau, J.T.F. & Fung, M. (1993) The Shatin Community Mental Health Survey in Hong Kong: Major Findings. Archives of General Psychiatry, 50, 125-133.
Chen, S.C.L. (1986) Child Psychiatric Cases Attending a Government Psychiatric Out-patient clinic over six years. In Mental Health in Hong Kong (ed.) T.P. Khoo. Mental Health Association of Hong Kong. pp.107-119.
Cheng, K.K., Leung, C.M., Lo, W.H. & Lam, T.H. (1989) Suicide among Chinese schizophrenics in Hong Kong. British Journal of Psychiatry, 154, 243-246.
Ewing, J.A. & Rouse, B.A. (1976) Failure of an experimental treatment program to inculcate controlled drinking in alcoholics. British Journal of Psychiatry, 124, 518-525.
Gelder, M., Gath, D. & Mayou R. (1984) Oxford Textbook of Psychiatry. Ch.13, pp.398-421.
Graham, P. (1979) Epidemiological studies. In Psychological disorders of childhood (ed) H.C. Quay & J.S. Werry. Wiley, New York.
Hong Kong Government (1991). Hong Kong 1990 Review of Rehabilitation Program Plan Health & Welfare Branch, Government Secretariat. Government Printer, Hong Kong.
Hung, S.F. (1993) Psychiatric services for autistic persons in Hong Kong. Journal of the Hong Kong College of Psychiatrists, 3, Suppl. 1, 8-12.
Kaplan, H.J. & Sadock, B.J. (1988) Synopsis of Psychiatry (5th ed.) Ch.29 Psychiatric Emergencies, pp.452457. Williams & Wilkins. Baltimore.
Lam, P. (1987) Morbidity in Hong Kong, 1985-6. The Hong Kong Practitioner, 9, , 2652-2666.
Lawson, , J.S. (1991) Public Health - Australia. School of Health Service Management. University of New South Wales. Sydney.
Lee, S.H. (1990) 1988-1989 Departmental Report. Director of Medical and Health Department. Government Press. Hong Kong.
Leung, S.P. (1991) Alcoholism - catching a tide of awareness. Journal of the Hong Kong College of Psychiatrists, 2, 15-20.
Leung, T.M. & Lo, W.H. (1984) Attempted suicide - study of hospital sample. Bulletin of the Hong Kong Medical Association, 36, 85-97.
Lo, W.H. (1982) Issues in psychiatric care of the elderly in Hong Kong. Journal of the Hong Kong Psychiatric Association, 2, 6-9.
Lo, W.H. & Leung, T.M. (1985) Suicide in Hong Kong. Australian and New Zealand Journal of Psychiatry, 19, 287-292.
Ma k, K Y. (1991) Future developments in community treatment for the mentally ill in Hong Kong. Journal of the Hong Kong Medical Association, 43, 2, 124-129.
Mak, K.Y. (1993) Hyperkinetic disorder - a public health point of view for Hong Kong. Journal of the Hong Kong College of Psychiatrists, 3, Suppl. 1, 22-26.
Mak, K Y. & Gow, L. (1992) The cost-benefits of an aftercare service for psychiatric patients discharged from half-way houses in Hong Kong. (Paper submitted for publication).
Mak, K Y. & Wong, M.H. (1988) Psychiatry in private practice in Hong Kong: Personal Viewpoints. Journal of the Hong Kong Psychiatric Association, 8, 12-17.
Mann, A.H., Jenkins, R. & Belsy, E. (1981) The twelve-month outcome of patients with neurotic illness in general practice. Psychological Medicine, 11, 535-550.
Miller, S. (1979) The Biosocial Survey in Hong Kong. Canberra, Australian National University.
Oyebode, F. (1994) Ethics and resource allocation: can health care outcomes be QALYfied? Psychiatric Bulletin, 18, 395-198.
Pan, P. C. (1989) Parasuicide in the elderly: A long neglected problem. Hong Kong Journal of Gerontology, 3, 2, 39-42.
Shepherd, M., Cooper, B., Brown, A.C. & Kalton, G. with new material for 2nd ed. by Shephard, M. & Clare, A. (1981) Psychiatric Illness in General Practice. 2nd ed. Oxford University Press. Oxford.
Shum, P.S. (1981) Alcohol, alcoholism and Hong Kong. In Aspects of Mental Health Care in Hong Kong (ed.) T.P. 1-Khoo. Mental Health Association of Hong Kong. pp.279-289.
Singer, K. (1972) Drinking patterns and alcoholism in the Chinese. British Journal of Addiction, 67, 3-14.
Street, J. (1986) New hope for mentally ill street sleepers. In
T.P. Khoo (Ed.) Mental Health in Hong Kong 1986, pp.83-87. Mental Health Association of Hong Kong. Hong Kong.
Tennant, F.S. & Hurry, J. (1981) The short-term outcome of neurotic disorders in the community: the relation of remission to clinical factors and to 'neutralizing' life events. British Journal of Psychiatry, 139, 213-20.
Williams, A. (1985) The value of QALYs. Health & Social Services Journal, XCIV, 495-497.
K.Y. Mak MBBS, MRCPsych, DPM, MHA Senior Lectu rer, Department of Psychiatry, The University of Hong Kong, Queen Mary Hospital, Pokfu /am Road, Hong Kong.