Hong Kong Journal of Psychiatry (1997) 7 (1), 3-8
SPECIAL TOPIC: Consultation-Liaison Psychiatry
Summary
The Consultation-liaison Team of Kwai Chung Hospital has collected data regarding the psychiatric service it provided to the in-patients of a nearby regional general hospital in the period between July 94 and June 95. The characteristics of the referrals were documented and discussed. Information on all the 968 consultations seen was collected in the following areas, namely, demographic data, source and reason of referral, past psychiatric and suicidal histories, current suicidal attempt, psychiatric diagnosis, significant medical problem, psychiatric outcome and number of session(s) provided. 77% of the total sample were from the department of medicine and 45% had a past psychiatric history. Suicide attempt was the commonest reason of referral, accounting for one-third of all referrals, while self overdosing was the method adopted by 44% of the suicide attempters. 41% of attempters were under 26 years old and 84% under 46 years old. Half of them, nonetheless, were not suffering from any formal psychiatric problems apart from adjustment disorders. Out of the 229 patients suffering from schizophrenia referred to us for assessment, 116 of them had no significant physical problem. Apart from describing the experience of a local service, this study also suggests in-patient treatment in general hospital may not be necessary for some suicide attempters and patients presented with schizophrenic symptoms.
Keywords: consultation-liaison psychiatry, Hong Kong, suicidal attempt, schizophrenia
INTRODUCTION
Consultation-liaison (C-L) psychiatry may be defined as a subspecialty of psychiatry, one concerned with clinical service, teaching, and research at the borderland of psychiatry and medicine (Lipowski, 1986), and its main goal is to bring medicine and psychiatry closer together so as to improve patient care in its psychosocial and psychiatric aspects. Lipowski (1986) reviewed the 50 years' history of C-L psychiatry in the United States and described its development as divided into four overlapping phases: the beginnings, the organizational phase, the phase of conceptual development, and the phase of rapid growth. However, the status of a subspecialty of psychiatry was only achieved in the country after 1970 (Lipowski, 1983).
In Australia, the history of C-L psychiatry was shorter and it only started in 1970s, under influence of the North American model of liaison psychiatry, with its emphasis on the biopsychosocial model and psychoanalysis. Anyway, the development of the subspecialty has been said to be slow in the country and variable in different hospitals (Smith et al., 1993). In the United Kingdom, its development has been even slower, despite recognition of deficiencies in psychiatric service offered to general medical units (Creed, 1991). The reasons behind include hesitation to alter current psychiatric practice and lack of resources. In Hong Kong, C-L psychiatry is not yet recognized as a subspecialty and only treated as a part of general adult psychiatry by the Royal College of Psychiatrists and the Hong Kong College of Psychiatrists.
KWAI CHUNG HOSPITAL C-L TEAM
Kwai Chung Hospital (KCH) is a mental hospital located next to a regional general hospital, Princess Margaret Hospital (PMH). It started its operation in 1981. Besides admitting psychiatric in-patients, the hospital also provided psychiatric consultation to PMH in-patients. All along, the duty was shared among general adult psychiatric teams. In 1994, a consultation-liaison team was established. It took over the duty of psychiatric consultation to PMH, except for patients under age of 16. Although a psychogeriatric team would take care of a proportion of patients in geriatric wards, the C-L team provided psychiatric consultation to the majority of elderly patients, without upper age limit, in various wards of PMH.
In 1994, the team comprised 1 consultant psychiatrist, 1 senior medical officer and 3 medical officers. However, the team only spent half of its time to provide consultation services to 3 general hospitals, including Princess Margaret Hospital , Caritas Medical Centre and Yan Chai Hospital.
The workloads of latter two were relatively small compared to that in PMH. These general hospitals with over 2500 beds did not have their own psychiatric unit.
All consultation referrals were initiated by the referring doctors of the 3 general hospitals. After receiving the referrals, they were assigned to the team members according to the reason of referrals and the likely psychiatric problems. There were 3 consultation-liaison rounds every week and every case seen by medical officer would be presented and discussed. Cases would be reassessed by the consultant or senior medical officer if needed, before or after consultation-liaison rounds.
A database of the consultation service was established soon after the establishment of the team. It served multiple purposes, including filing and quality assurance. It contained information about patient's demographic data, source and reason of referral, past psychiatric and suicidal histories, current suicidal attempt, psychiatric diagnosis, significant medical problem, psychiatric outcome and disposal, as well as number of session provided. Every patient referred for psychiatric consultation would have a record after the case was discussed. A data input form {Appendix) would be completed by the case doctor and double checked before entering into a computer database programme.
OBJECTIVE
This paper examined the consultation services to PMH for the period from 1July 94 till 30 June 95. It was the first year of the C-L team. However, the data collected actually reflected what KCH had been doing in the previous 13 years and carried to the C-L team. The data revealed the demand from the general hospital and might disclose the deficiency of the consultation services. In other words, it would be a reference for the future development of C-L psychiatry in the region.
METHODOLOGY
All records of PMH referrals from 1 July 94 to 30 June 95 were extracted from the database and divided according to 4 sources of referral: medical (including geriatric), surgical, obstetric & gynaecology (0 & G) and orthopaedic.
The patients' demographic data, source and reason of referrals, past psychiatric and suicidal histories, current suicidal attempt, psychiatric diagnosis, significant medical problem, psychiatric outcome as well as number of session provided were analyzed accordingly.
OVERVIEW
RESULTS
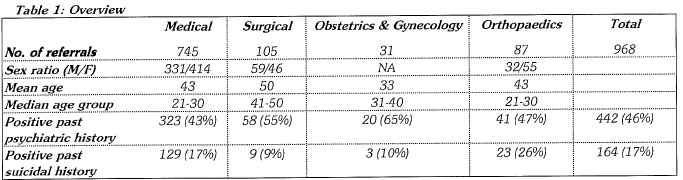
As shown in Table 1, altogether there were 968 psychiatric consultation referrals from PMH in the year, and about three quarters came from medical units. 45 % of all referrals had definite past psychiatric history. In medical and orthopaedic units, patients of early adulthood were the major target group of the consultation activities. However, there were also a significant proportion of elderly patients referred to the team, and so the marked difference between the median age and the mean age was shown in the two units.
REASON OF REFERRAL
Suicide assessment was the commonest reason of psychiatric consultation and accounted for about one-third of referrals from medical, surgical and orthopaedic units. However, in medical units, besides 240 (32.2%) referrals for suicide assessment, psychosis and related reasons (such as violent tendency, confusion and abnormal behaviour or mood) accounted for the other 212 (28.5%) referrals. In Surgical, Orthopaedic and O&G departments, assessment of mental capacity to consent was one of the major tasks (37 cases, 16.6%), while postpartum psychiatric assessment was the most frequent request (25%) from O&G Department. However, psychiatrist's opinion about termination of pregnancy (TOP) was rarely asked for.
Altogether, there were 58 (6.0%) out of 968 cases referred for the reason of depressed mood. Neurotic and somatic symptoms were infrequently quoted as the main reason for psychiatric consultation, and only accounted for 25 (2.6%) and 16 (1.7%) cases respectively. Revision of psychiatric drugs was asked for in 23 cases (2.4%) and most were concerned with side effects of antipsychotics or tricyclic antidepressants.
Some referring doctors requested psychiatric consultation by giving unclear or non-specific reasons, such as "routine assessment", "psychiatric assessment" or "past history of psychiatric problem" etc. It gave rise to about 20% of all referrals. Furthermore, there was a small proportion having rather distinct reasons of referral that could not be classified into the major groups.
PSYCHIATRIC DIAGNOSIS
Every consultation case was given 1 to 2 clinical diagnoses according to ICD 10 Classification up to the third digit. The first or the main diagnosis was referring to the one most relevant to the reason of referral and the clinical presentation of that particular admission. The psychiatrist was allowed to enter 2 diagnoses at most.
Altogether, 99 (10.2%) patients were given organic mental disorders as the main diagnosis, including 46 dementia and 37 delirium. Eighty-one (8.3%) were suffering from mental disorders due to psychoactive substance use. Among them, 42 were related to alcohol use. There were 241 (24. 9%) patients suffering from functional psychosis other than mood disorders, including 169 schizophrenia, 38 acute schizophrenia-like psychotic disorder and 22 delusional disorder. One hundred and two (10.5%) patients had mood disorders, including 50 depressive episode and 29 manic episode or bipolar disorder. Forty-one (4.2%) patients suffered from neurotic disorders, such as phobic & anxiety disorders (10 cases) and dissociative disorders (10 cases). Besides, there were 205 (21.2%) patients having diagnosis of reaction to stress, adjustment disorder or problems due to psychosocial circumstances. Thirty-eight (3. 9%) patients were given no psychiatric diagnosis after seen and 112 (11.6%) could not be given any definite diagnosis as most of them were discharged before seen by psychiatrist.
Out of 968 patients, 68 were given more than one psychiatric diagnosis. Concerning the second psychiatric diagnosis, personality disorder (21 cases) and mental retardation (10 cases) were the commonest two.
SUICIDAL ATTEMPT AND RELATED ISSUES
Out of 968 referrals, 312 patients presented with "suicidal" behaviour, including 107 males and 205 females. In other words, the approximate male to female ratio was 1 to 2, with greater discrepancy of 1to 2.4 for the age group of 16-25 years old. Also, the majority of suicidal attempters belonged to the younger age groups that 129 (41%) and 133 (42.6%) were of age group 16-25 and 26-45 respectively. There were only 28 (9.0%) and 22 (7.1%) patients belonged to age group of 46-65 and above 65 respectively. Among these suicidal patients, 84 had definite past psychiatric history and 110 had previous suicidal attempts.
The psychiatric diagnosis most frequently made for this group of patients was reaction to stress, adjustment disorder or problems related to psychosocial circumstances, which accounted for 156 cases (50%). Besides, schizophrenia and related psychotic conditions (39 cases, 12.5%), depressive disorders (31 cases, 10.0%) and mental disorders due to psychoactive substance use (14 cases, 4.5%) were the next commonest diagnoses. However, 49 cases (15.7%) got deferred diagnosis as they were discharged before psychiatric assessment.
Concerning methods of suicidal attempt, drug overdose was most frequently used and accounted for 137 out of 312 cases (43.9%). Wounding (71 cases, 22.8%) and ingestion of corrosives or detergents (38, 12.2%) were the next two commonest methods. Nineteen (6.0%) suicide attempters used more than one method at one time, and the commonest combination was drug overdose and wrist cut. Among violent methods, including gas poisoning, jumping from height, hanging, drowning, shooting, falling in front of moving vehicle and crashing car etc., jumping from height was the commonest one. It accounted for 17 cases and was equivalent to 5% of all cases of suicidal attempt. There was no record of suicidal attempt by gun shot during the year.
SCHIZOPHRENIA & RELATED PSYCHOTIC DISORDERS
Altogether, there were 229 referrals given schizophrenia or related psychotic disorders as the primary diagnosis in the total sample. Out of them, 160 (70.0%) had past psychiatric history and 66 (28.8%) had none, while three were uncertain. One hundred and three (45.0%) were suffering from significant physical illness, which might be the main reason of the hospitalization. Reasons of psychiatric consultation included "routine" assessment due to past history of psychosis, assessment of mental capacity for consent, and postpartum psychiatric assessment. Ten other patients were suffering from side effects of psychiatric medication and psychiatrists were asked to revise treatment. However, 116 (50.7%) of this group of psychotic patients did not have any significant physical illness and they were mainly admitted to the general hospital for psychiatric assessment and management.
Concerning the further psychiatric management, 114 patients (50.0%) were transferred to KCH for in-patient care and 88 (38.4%) were referred to out-patient psychiatric centre. Out of the 229 patients, 5 with definite past history of schizophrenia were discharged before seeing psychiatrist and 9 were discharged against medical advice of mental hospital admission after psychiatric consultation.
DELIRIUM & MEDICAL PROBLEM
Altogether, there were 37 cases of delirium out of 968 referrals. Nearly all cases had significant physical illness, except 2 cases for whom organic aetiology were not certain. Among the 37 cases, 3 got significant physical problem in multiple systems, 11 involved central nervous system (8 out of 11 cases were epilepsy) and 8 cases had urinary tract problem (including urinary tract infection and renal failure).
Out of these 37 patients, 4 were found to have underlying dementia. The mean age was 57 but two thirds were above 60 years old. Concerning the further psychiatric management, only 1 case was admitted to KCH, 13 were referred to out-patient and the rest did not need further psychiatric management.
TERMINATION OF CONSULTATION AND FURTHER MANAGEMENT
Out of 968 cases referred for psychiatric consultation, 89 (9.2%) were discharged before seen by psychiatrist and 12 (1. 2%) were cancelled. Two-third of patients (646 cases) were seen by psychiatrist once only, and about 200 cases (20.7%) needed more than one session of management. On average, after excluding the cancelled referrals, each referral was spent with 1.4 session. After seen, 189 patients (22%) were admitted to Kwai Chung Hospital for further management, and 23 (3%) cases were advised in-patient management but discharged against medical advice. Four hundred and seventeen patients (48%) were referred to outpatient psychiatric centres and a minority (6%) were ref erred to private psychiatrists, social services or other psychiatric institutes. 157 patients (18%) did not need further psychiatric follow up.
DISCUSSION
DEVELOPMENT OF CONSULTATION-LIAISON PSYCHIATRY IN HONG KONG
C-L psychiatry in Hong Kong is still at an early stage of development, equivalent to the beginnings or, at most, early organizational phase of its development in the USA. In Hong Kong, the workload of psychiatric consultation is heavy. It is estimated that each full-time doctor, on average, needs to take care of about 500 referrals per year. It is based on the KCH C-L team's experience during the year that a team of 5 doctors (1 consultant, 1 senior medical officer and 3 medical officers) spent half of their working hours to provide C-L psychiatric services to about 1250 referrals in 3 general hospitals. Besides suicidal assessment and management of adjustment disorder or related problems, the C-L team's major workload was the care of patients with major psychoses admitted to general hospitals. These two major arenas of job would remain C-L services' bread and butter.
There is still little emphasis in the interface between physical and mental health, concerning the current practice of C-L psychiatry. In the year, there were only 16 referrals quoted with somatic symptoms as the main reason of psychiatric consultation. Some patients with significant physical illness might have adjustment problem or depression, but they were usually not referred until gross depression or having suicidal intent. It might reflect the physician's low awareness of psychiatric morbidity among physically ill patients. In the USA, the prevalence of psychiatric morbidity in the hospitalized medically ill was estimated to be between 10% to 50% (Popkin, 1995). Their experience showed that better liaison between the C-L psychiatrist and various departments in general hospital could significantly shorten the length of stay in general hospital. This area would be the target of development and certainly the patients could benefit from it. Also, it fits the principle of cost-effectiveness, which is pursued by every comptroller of hospitals. Renal dialysis units, intensive care units and coronary care units would be the sites of the C-L activities, besides general wards. Maybe, following the trends in the USA, with technological advance in medicine the focus of C-L psychiatry will shift to transplantation units' haematology and oncology units as well as acquired immune deficiency syndrome (AIDS) treatment centres.
As mentioned above, a significant proportion of referrals to the C-L team had no significant physical problem. These patients might not need the stays in general hospital, if psychiatric consultation could be offered immediately or within a short time. The solution may be psychiatric consultation in Accident & Emergency Departments (A&E) instead of only in general wards. The present study found that there were at least 116 patients with psychotic conditions and no significant physical condition admitted to PMH within the year. Also, 156 out of 312 patients presented with suicidal attempt were having adjustment disorder or related conditions. They might only need psychiatric assessment and counselling in A&E or outpatient psychiatric centre. In other words, it is estimated that more than 200 general hospital admissions per year could be saved or at least reduced in length of hospital stay, if C-L psychiatric service was provided in A&E. Then, those patients could have psychiatric assessment and management without unnecessary delay. However, the cost of the service would be a full time experienced psychiatrist on demand to see the referrals from A&E.
Besides in-patient psychiatric consultation-liaison work C-L team should also take care of out-patients with psychosomatic problems, which may be best done by close liaison with physicians. Sexual dysfunctions, sleep disorders and pain conditions are examples, although there would be some overlaps with general adult psychiatry.
Proactivity and inter-activity are the characteristics of C-L psychiatry. Prevention and early intervention of psychiatric morbidity are also the duties of C-L psychiatrists, including education to staff of various departments about psychiatric morbidity in their wards. C-L psychiatrists' effort in perinatal psychiatric care may demonstrate these characteristics of the sub-specialty, where psychiatric morbidity is high during post-partum period. With the cooperation of obstetricians they may have opportunities to educate pregnant women; and staff. Then the pregnant women would have good psychological preparation towards the changes during perinatal period, while the staff would have raised alertness towards the perinatal psychiatric morbidity. It is to be hoped that swift intervention can be offered for conditions like perinatal loss and postpartum psychosis. Also postpartum depression can be detected and intervened without delay.
SUICIDAL ATTEMPT AND ASSESSMENT
Assessment of suicidal risk is a major task of every psychiatrist. However, C-L psychiatrists particularly spent more time in suicide assessment and for patients without formal psychiatric illness outside psychiatric settings. Many patients with 'suicidal attempt' or 'parasuicide' presented to general hospital are otherwise physically and mentally healthy. They may regard psychiatric assessment a stigma and may refuse to see psychiatrist or disclose their information. Also, the underlying intents of the "suicidal attempt" are various. Some patients really intend to kill themselves but are prevented by their ignorance of lethality of methods or by chance intervention by others. Some may have other intents, such as seeking an interruption in an undurable state of tension. Some parasuicidal acts may represent the 'cry for help', while some are carrying hostility and trying to make others around them feel guilty or anxious. Some acts are testing the benevolence of fate, instead of having clear intention of their acts (Kreitman, 1993).
Concerning methods of suicidal attempt, drug overdose was the commonest in our study, while wrist cut and ingestion of corrosive or detergent were the next two commonest ones. Although many suicide attempters with these methods are usually regarded as having minor emotional turmoil and low risk of suicide, the attempts should not simply be regarded as not genuine and of low suicidal risk. However, other suicidal methods such as gas poisoning, jumping from height, hanging, drowning, shooting, falling in front of moving vehicle and crashing car should be treated more seriously as they carry high suicidal risk.
DELIRIUM AND MEDICAL PROBLEMS
During the whole year, among 968 psychiatric consultation referrals, there were only 37 patients diagnosed to have delirium, excluding those secondary to alcohol or other substance misuse. Certainly, this only reflected the pattern of referral, instead of genuine number of cases occurring in the year. The incidence might be much higher and they might be transient and recovered spontaneously.
However, some cases referred to psychiatrists might be those suspected to be functional psychotic conditions by the physicians, or the problems had been prolonged. Then, it might suggest CNS problems, especially epilepsy, and urinary tract problems were frequently unrecognized aetiologies of delirium.
There might be a small proportion of elderly delirious patients referred to psychogeriatric team and they might not be included in the present study. However, the number would be small as the psychogeriatric team only provided ward consultation to geriatric wards on weekly basis in the year, unless the geriatricians got different pattern in making referral to the team.
EFFICIENCY AND DISCHARGE BEFORE PSYCHIATRIC ASSESSMENT
Ten percent of total number of referrals were discharged before psychiatric assessment and usually the referring doctors were not willing to do so. Instead, the patients ref used to wait for the assessment. Most of them were referred for suicide assessment, but there was a small proportion suffering from psychotic conditions and could not be kept in the ward by the staff . One of the factor was that the waiting time was unnecessarily prolonged. In a separate study (Ku, 1995, unpublished data) on the efficiency of the consultation service to PMH during the period from November 94 to April 95, it was found that only 50% of referrals could reach the C-L team within 24 hours and about 20% took more than 48 hours. However, 90% of referrals could be dealt with by the psychiatrists within 24 hours upon receiving the referral. It is to be hoped that the waiting time for psychiatric consultation would be markedly shortened by upgrading the priority of the C-L service and sending referrals by facsimile. Then the rate of discharge against medical advice could be decreased and the patients could get swift and proper psychiatric assessment and care.
CONCLUSION
The establishment of a consultation-liaison psychiatric team indicates the change of psychiatrist's role in a general hospital: adopting a proactive or interactive attitude towards the psychiatric morbidity in general hospital patients, rather than a passive one. Management of suicide attempters and schizophrenic patients will continue to be the major tasks of a C-L psychiatric team in Hong Kong. Swift C-L service will reduce the length of stay in general hospitals. However, the present study is a retrospective and descriptive one. A control study is needed before one can reach the conclusion that provision of C-L psychiatric service can shorten length of hospital stay and improve the cost-effectiveness of the whole hospital operation.
Concerning training programme for a trainee psychiatrist, consultation-liaison psychiatry should be a mandatory part of the whole scheme, as assessment and management of suicidal attempt are essential clinical skills. Also, the psychiatric morbidity in general hospital is distinct and different from that in psychiatric settings.
REFERENCES
Creed, F. (1991) Liaison psychiatry in the 21st century - a review. Journal of the Royal Society of Medicine, 8: 414-417.
Kreitman, N. (1993) Suicide and parasuicide. In: Kendell R.E. & Zealley A.K., (ed.) Companion to psychiatric studies, 5th edition. pp. 743-760 Churchill Livingstone, Edinburgh.
Lipowski, Z.J. (1983) Current trends in consultation-liaison psychiatry. Canadian Journal of Psychiatry, 28: 329-338.
Lipowski, Z.J. (1986) Consultation-liaison psychiatry: the first half century. General Hospital Psychiatry, 8: 305-315.
Popkin, M.K (1995) Consultation-liaison psychiatry. In: Kaplan, H.J. & Sadock, B.J., (ed.) Comprehensive Textbook of Psychiatry, 6th edition. pp. 1592-1605 Williams & Wilkins, Baltimore.
Smith, G.C., Ellis, P.E., Herrman, H.E. (1993) Consultation Liaison Psychiatry in Australia. General Hospital Psychiatry, 15: 121-124.
*Ku Kwok-hung MBChB, MRCPsych Senior Medical Officer, Consultation-liaison Team, Kwai Chung Hospital
Nguyen Desmond Gia-hung MBBS, MRCPsych Senior Medical Officer, Consultation-liaison Team, Kwai Chung Hospital
Ng Yin-kwok MBBS, MRCPsych, FHKAM (Psychiatry) Chief of Service, Consultation-liaison Team, Kwai Chung Hospital
*Correspondence; Dr. Ku Kwok-hung, Senior Medical Officer, Consultation-liaison Team, Kwai Chung Hospital, 3-15 Kwai Chung Hospital Road, Kwai Chung, Hong Kong.



