Hong Kong Journal of Psychiatry (1997) 7 (1), 3-8
SPECIAL TOPIC: Consultation-Liaison Psychiatry
Summary
The emphasis on the community care of psychiatric patients has led to, inter alia, the development of general hospital psychiatric units. After a review of the overseas and local histories, the particular roles of the general hospital psychiatrist are discussed and some suggestions are made for the future development of general hospital psychiatry in Hong Kong.
Keywords: psychiatry, general hospital, Hong Kong, consultation-liaison, re-integration
INTRODUCTION
There is a recognized international trend towards managing mental patients in the community as far as possible. One of the results has been the development of psychiatric units in general hospitals while mental hospitals are seldom or no longer built. In Hong Kong, the policy of the Hospital Authority (a statutory quasi-governmental body established on 1 December 1990 to manage all local public hospitals) is in line with this (Hong Kong Hospital Authority, 1995).
The benefits of community-based psychiatric care are certainly multiple. General hospital psychiatric units contribute substantially to the success of community-based care. This paper aims at reviewing the development of general hospital psychiatry in Hong Kong, looking at this aspect of our practice in relation to the whole specialty and discussing some particular roles of the general hospital psychiatrist.
PSYCHIATRIC SERVICE FOR THE GENERAL HOSPITAL PATIENTS
Three models are discernible when we consider how the general hospital patient gets psychiatric care.
They may be referred to the psychiatric clinics just like patients requiring the attention of doctors of any other specialty. A considerable proportion of these have to be seen quickly. Many psychiatric out-patient departments reserve a number of urgent new case slots for such patients.
In the second model, visiting psychiatrists go to the general hospital wards to see the patients. Being visitors, the psychiatrists have no offices of their own and often have to assess the patients under circumstances not entirely suitable.
If there is a psychiatric unit within the general hospital itself, flexibility with respect to the time and place of the consultation or assessment will be enhanced. There is also increased sophistication of the service.
In general, these models have developed in a chronological order. As we go from the first model to the third, there is progressive integration of the psychiatric and non-psychiatric aspects of patient care and the service becomes more and more client-centred. However, all three modes of service delivery still exist to different extents in various parts of the world including Hong Kong.
HISTORY
OVERSEAS PICTURE
All over the world before the 1950s, the single word that could describe the policy of managing mentally deranged individuals was "isolation". The psychiatrically ill were rejected and the "healthy" members of the community tried all means to separate them from the rest of the population. Wealthy families built extensions of their premises to accommodate mentally disordered relatives. Society at large put the less well-off psychiatric patients into asylums.
Lieh Mak et al (1981) provided a good summary of the development in the past 4 decades or so. The segregationist approach was increasingly challenged about 10 years after the second world war. While Thomas Szasz (1961) and R D Laing (1965) are perhaps the most well-known among the theoreticians of the anti-psychiatry movement in general, Maxwell Jones (1952), Russel Barton (1959), Erving Goffman (1961) and Franco Basaglia (1968) particularly opposed the method of managing mental patients prevailing then. Their efforts were greatly helped by the timely discovery of chlorpromazine and other antipsychotic drugs that offered considerable symptomatic relief to psychotic individuals (Kane & Freeman, 1994).
In the United Kingdom, the 1959 Mental Health Act provided the legal basis for the treatment of mental patients in non-psychiatric hospitals. By 1970, there were 106 general hospital psychiatric units. In North America, 1 in 11 general hospitals had a psychiatric unit in 1963. Within 8 years, the proportion increased to 1 in 7 (Lieh Mak et al, 1981). The Italians were more drastic. Law 180 was passed in 1978. Besides other provisions, it stipulated the establishment of psychiatric units of 15 beds or less in general hospitals. After May 1978, no first admissions to mental hospitals were allowed and after December 1981, any admission to these would be illegal. All patients requiring any form of psychiatric hospitalization, voluntary or compulsory, must be admitted to general hospital psychiatric units instead (Tansella & Williams, 1987).
Hence, at least in many developed countries, general hospital psychiatric units have burgeoned in one way or another in the past 4 or 5 decades. Decision-makers worldwide are naturally making adjustments where necessary and appropriate, but the trend appears undeniable.
LOCAL SCENE
The early situation in Hong Kong was largely the same. Before the opening of a temporary asylum on Hollywood Road in 1875, mental patients had been kept in a prison! After relocation, merging and expansion on several occasions in the following decades, Victoria Mental Hospital came into being on High Street in 1925 (Castle Peak Hospital, 1996; Lo, 1981). General hospital patients requiring psychiatric assessment were brought to the few clinics of the former Mental Health Service. The very occasional patient, such as a private case, was seen by the psychiatrist in the general hospital. In 1962, Queen Elizabeth Hospital Psychiatric Clinic was set up. It was open for not more than a few sessions per week and manned by psychiatrists from Castle Peak Hospital, the new mental hospital in the territory which gradually led to the closing of the asylum on High Street. The clinic operated until 1994.
In 1971, the first two general hospital psychiatric units were set up, one on each side of the harbour, at Queen Mary Hospital (the University Psychiatric Unit of University of Hong Kong) and Kowloon Hospital. The same took place three years later at United Christian Hospital, a subvented hospital at that time.
In 1975, Kowloon Hospital Psychiatric Unit doctors began consultation service at Queen Elizabeth Hospital. Six years later, the same service at Princess Margaret Hospital was provided by doctors from Kwai Chung Hospital, which was newly commissioned as the second mental hospital in the territory. In 1984, the Department of Psychiatry, Chinese University of Hong Kong was formally established at Prince of Wales Hospital. In 1991, Kwai Chung Hospital psychogeriatricians commenced consultation service at Kwong Wah Hospital. In the same year, the Mental Handicap Unit at Tuen Mun Hospital was set up. Ward consultation service at Tuen Mun Hospital was started in 1992 by doctors from Castle Peak Hospital. In the same year, the Department of Psychiatry of Shatin Hospital came into being. The same happened at Tuen Mun Hospital in 1993. Ward consultation service at Kwong Wah Hospital was expanded to all cases by Kowloon Hospital doctors in 1994, while Castle Peak Hospital colleagues began the same service at Pok Oi Hospital, and Kwai Chung Hospital staff offered Yan Chai Hospital and Caritas Medical Centre regular ward consultations. The Department of Psychiatry of Pamela Youde Nethersole Eastern Hospital also began its activities in 1994. Consultation service at Ruttonjee Hospital was started. Table 1 summarises the development of general hospital psychiatry in Hong Kong.

LOCAL GENERAL HOSPITAL PSYCHIATRY IN PERSPECTIVE
According to Lloyd (1980), liaison psychiatry denotes a style and location of practice rather than a discrete subspecialty. Consultation-liaison is one of the integral parts of general hospital psychiatry. Lloyd's view is, therefore, at least partly relevant to the present discussion.
Table 2 is an attempt to conceptualize the "where" and "whom" of psychiatric practice. Different groups of our clientele give rise to our subspecialties. The location of our service constitutes another dimension and the general hospital is one item in this. The number of crosses in each cell denotes the author's personal reckoning of the present state of development in terms of clinical activity volume. There is no judgmental element as to whether the situation is satisfactory or not.
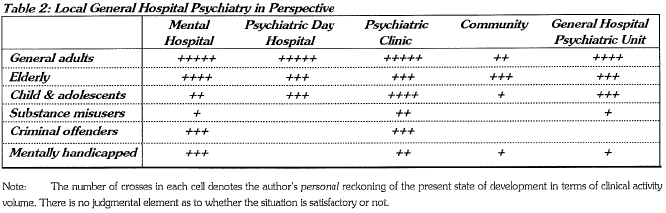
Many acute general hospitals in Hong Kong are now served by their own psychiatric departments. Most of the others receive regular consultation-liaison support from psychiatric institutions nearby. Other subspecialist care is available in most of the general hospital psychiatric units. Services for the elderly and for the children and adolescents are quite well developed, whereas those for the mentally handicapped and the substance misusers are less prominent, and that for the criminal offenders is virtually non-existing. In general, university-based general hospital psychiatric units offer a wider range of subspecialties.
PARTICULAR ROLES OF THE GENERAL HOSPITAL PSYCHIATRIST
While the following objectives should be shared by every psychiatrist irrespective of orientation or subspecialty, the general hospital psychiatrist, probably because of his or her major place of work, may achieve them more easily.
DE-STIGMATIZATION & PUBLIC EDUCATION
Stigmatization of the mental patient is still widespread despite some progress made recently in this connection. Much of the stigmatization sterns from unfamiliarity, or outright ignorance, leading to fear. As in phobia, avoidance of the dreaded object only reinforces the trepidation and hence the rejection.
General hospitals are, on the whole, physically much closer to the community than psychiatric ones. Hence, general hospital psychiatric units enjoy a distinct geographical advantage in facilitating the re-integration of the mentally ill into society. The various (in-patient, daypatient, out-patient and outreach) aspects of psychiatric service are more easily integrated: exactly the same team of professionals can manage the patient in different treatment settings, which are in close proximity to each other and, usually, to the patient's home.
Furthermore, many patients and relatives perceive less stigma attached to admission to a general hospital psychiatric ward. This enhances willingness to receive in-patient treatment and reduces psychiatric morbidity apparent to the lay public, and, in tum, serves to improve the mental patient's image.
The general hospital psychiatrist is also at an advantage in rendering education to the public on the multiple (biological, psychological and social) factors involved in health and sickness, thereby improving their understanding of mental illnesses and reducing their irrational fear of psychiatric patients.
IN RELATION TO NON-PSYCHIATRIC COLLEAGUES
Considerable difficulties still exist in the interaction between the psychiatrist and other clinicians. One reason is the adherence to the strict medical model by some non-psychiatric colleagues. As psychiatrists, we certainly understand the complex interplay of biological, psychological and social elements in health as well as sickness. Unfortunately, quite a few of our non-psychiatric colleagues do not share this insight. Therefore, apart from providing support in the form of achieving satisfactory control of patients' mental conditions so that proper treatment for their physical illnesses can be rendered, the psychiatrist should also contribute to the holistic care of patients in a more subtle, but perhaps more important, way. He or she should, during the consultation-liaison work, try to enable the non-psychiatric colleagues to obtain a more balanced view of the multiple factors involved in ill health. The general hospital obviously offers a geographically expedient location to do this.
By the same token, undergraduate students as well as postgraduate trainees can more easily grasp the holistic approach to management in the psychiatric department of a general hospital. This applies not only to medical, but also to nursing and allied health or paramedical professionals. After all, the division into clinical departments or specialties is arbitrary rather than natural.
RE-INTEGRATION INTO MAINSTREAM MEDICINE
It is also incumbent upon the general hospital psychiatrist to promote the re-integration of psychiatry into mainstream medicine. The long segregation of psychiatry from the rest of medical practice has produced a subtle dichotomy between psychiatric and "general" health care, not only perceived by the public, the policy makers and nonpsychiatric health care workers, but also ourselves! If this situation is considered unsatisfactory, everybody in our specialty, but perhaps particularly the general hospital psychiatrist, because of his or her strategic position, should contribute to its rectification. When this undue dichotomy is removed, stigmatization of the mental patient will also diminish and the re-integration of the mentally ill into society can be facilitated.
How, then, can the psychiatrist help in this campaign? Opportunities abound in the general hospital for more proactive efforts to collaborate with other clinicians. Offering our contribution to the management of a greater range of problems will be a key move. Many patients in general hospitals have under-diagnosed and under-treated psychiatric disorders, presenting as "mild" or "understandable" depression, or as somatic or "functional" complaints for which definite physical causes cannot be found. They may consume a lot of health care resources (Levenson et al, 1990). If they can be properly identified and treated, multiple parties will benefit. Setting up "Combined Pain Clinics" with, say, physicians and/or anaesthetists may be considered. Conducting joint-department case conferences with specialties that often consult us (such as the Medical and the Accident & Emergency Departments) has served to foster mutual education and establish a nonthreatening communication channel. General hospital psychiatric patients inevitably come into frequent contact with the staff of other departments. Many of the latter do find the interaction worrying. Talks on the handling of psychiatric patients (particularly those with violent propensities) and on the administration of physical restraint as well as its monitoring have been well received. On the more form.al front, active participation in hospital-wide projects like anti-smoking campaigns, open days and training courses for interns has been very fruitful. Compiling guidelines for non-psychiatric colleagues on commonly encountered problems such as the decisionmaking process for mentally incompetent patients has been tried with success.
FUTURE DEVELOPMENT IN HONG KONG
Several new psychiatric institutions will come into being in the next few years in Hong Kong. Each of the new general hospitals (Alice Ho Miu Ung Nethersole Hospital, North District Hospital and Tseung Kwan O Hospital) will include a psychiatric department. Kowloon Hospital and United Christian Hospital will have their existing departments considerably expanded.
With the establishment of more and bigger psychiatric departments within both old and new general hospitals, more emphasis may be put on liaison. The psychogeriatricians and child and adolescent psychiatrists are already collaborating closely with the corresponding physicians. Other efforts, such as those suggested in the previous section, may be worth considering.
CONCLUSION
The psychiatric hospital has been our fiefdom (Kendell, 1996). The 2 mental hospitals in Hong Kong are playing immensely important roles in psychiatric care delivery and will continue to do so. Despite what has happened in some places, they will and should not be closed, at least in the foreseeable future, because of our unique social, cultural, historical and political situation. Too drastic changes have proven to be undesirable elsewhere. We just have to diversify in some way. Further development of general-hospital-based psychiatric service is one of the likely trends.
REFERENCES
Barton, W. R. (1959) Institutional Neurosis. Bristol: Wright. Basaglia, F. (1968) L'Istituzione Negata. Turin: Einaudi.
Castle Peak Hospital (1996) Commemorative Volume for the Thirty-fifth Anniversary of Castle Peak Hospital. Hong Kong: Castle Peak Hospital.
Goff man, E. (1961) Asylums: Essays on the Social Situation of Mental Patients and Other Inmates. New York: Doubleday.
Hong Kong Hospital Authority (1995) Annual Plan 1995-1996. Hong Kong: Hong Kong Hospital Authority.
Jones, M. (1952) Social Psychiatry: a Study of Therapeutic Communities. London: Tavistock.
Kane, J. M. & Freeman, H. L. (1994) Towards more effective antipsychotic treatment. British Journal of Psychiatry, 165 (suppl. 25), 22-31.
Kendell, R. E. ( 1996) Introducing the new President, Professor R. E. Kendell. Psychiatric Bulletin, 20, 385-386.
Laing, R. (1965) The Divided Self. Harmondsworth: Penguin.
Levenson, J. L., Hamer, R. M. & Rossiter, L. F. (1990) Relation of psychopathology in general medical inpatients to use and cost of services. American Journal of Psychiatry, 147, 1498-1503.
Lieh Mak, F., Tam, Y. K., Yu, K. K., et al (1981) Psychiatric unit in a general hospital. In Aspects of Mental Health Care Hong Kong 1981 (ed. T. P. Khoo), pp. 57-66. Hong Kong: Mental Health Association of Hong Kong.
Lloyd, G. G. (1980) Editorial: whence and whither 'liaison' psychiatry? Psychological Medicine, 10, 11-14.
Lo, W. H. (1981) Government Mental Health Service. ln Aspects of Mental Health Care Hong Kong 1981 (ed. T. P. Khoo) Hong Kong: Mental Health Association of Hong Kong.
Szasz, T. S. (1961) The Myth of Mental Illness. New York: Haeber-Harper.
Tansella, M. & Williams, P. (1987) Editorial: the Italian experience and its implications. Psychological Medicine, 17, 283-289.
W. N. Orlando Tang MBBS, MRCPsych, FHKCPsych, FHKAM(Psychiatry) Chief of Service & Consultant, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, 3 Lok Man Road , Chai Wan, Hong Kong.


