Hong Kong J Psychiatry 2002;12(2):20-24
CASE REPORT
KK Wu
Acknowledgements: I would like to thank Dr Fung Yiu Wah for the medical information of the case reported, Dr Karen Shum and Ms Sumee Chan for their valuable advice. Also thanks to Mr Tsang Wai Ming for his clerical assistance.
KK Wu, MSocSc (Clin Psych), MAPS, AFHKPS, Department of Clinical
Psychology, Caritas Medical Centre, Hong Kong
Address for correspondence: Dr KK Wu, Department of Clinical Psychology, Caritas Medical Centre, 111 Wing Hong Street, Shamshuipo, Kowloon, Hong Kong
Tel: (852) 3408 7975
Fax: (852) 2307 5894
E-mail: wukyk@ha.org.hk
Submitted: 26 September 2001; Accepted: 28 January 2002
Abstract
This case report illustrates the utilisation of eye movement desensitisation reprocessing for treating a patients with post-traumatic stress disorder after a motor vehicle accident. Standardised measurements (Hospital Anxiety and Depression Scale and Impact of Event Scale-Revised) were adopted to monitor treatment effectiveness during various treatment phases. This case demonstrates the possible application of eye movement desensitisation reprocessing for the Chinese population and the treatment efficacy of eye movement desensitisation reprocessing for post-traumatic stress disorder. The implications for future research are discussed.
Keywords: Eye movement desensitization reprocessing, Motor vehicle accident, Post-traumatic stress disorder, Treatment effectiveness
Introduction
Eye movement desensitisation and reprocessing (EMDR) was developed by Shapiro1,2 as a new method for treating post-traumatic stress disorder (PTSD). In brief, EMDR involves eliciting rhythmic, bilateral eye movements from the patient. During this movement, the patient is asked to visualise an image related to the traumatic memory while internally repeating the negative self-statement associated with the memory. Throughout this process, the emotional and physiological arousal originally associated with the memory is desensitised.
The next treatment phase involves installation of posi- tive self-statement, which is then followed by reduction of body tension associated with the trauma. EMDR is completed as the dysfunctional impact of psychological trauma is reprocessed, and the positive self-statement becomes totally valid to the person.
The theoretical underpinning of EMDR is mainly hypothetical. An accelerated information-processing model was used as a working hypothesis to guide the use of EMDR.3 According to this model, a severe psychological trauma will lead to changes in the nervous system in patients with PTSD. Thus, the information acquired at the time of the traumatic event, including images, sounds, affect, and physical sensations, is neurologically maintained in its disturbing state.
The original material, which is held in this distressing state, continues to be triggered by a variety of internal or external stimuli and is expressed in the form of intrusive thoughts, avoidance behaviour, and increased arousal. The eye movements (or alternative stimuli) used in EMDR trigger a physiological mechanism that activates the information- processing system.
The mechanisms proposed for this activation include the dual focus of attention for both the past trauma and alternative stimuli, a differential effect of neuronal burst caused by the various stimuli, and deconditioning caused by a relaxation response. The main assumption of EMDR is that activating the processing of the trauma memory will naturally enhance adaptability and lead to resolution. Thus, borrowing the hypothesis of the information-processing system, EMDR is conceptualised as working through memory networks. When using EMDR, it is necessary to ‘clean out’ each associative channel of a target traumatic memory for example, images, sounds, and affect by repro- cessing all of the dysfunctionally stored material connected to the target.
According to a project initiated by the American Psychological Association Division 12 (Clinical Psychology) to determine the degree to which therapeutic methods were supported by solid empirical evidence, EMDR was placed by independent reviewers on a list of “empirically validated treatments” as “probably efficacious for civilian PTSD”. The other treatment methods listed as “probably efficacious for PTSD” only include exposure therapy and stress inoculation therapy.4 Despite the rising popularity of EMDR as a treatment for PTSD in the West and the research evidence accumulated, there is a lack of case reports or study of the technique in the Chinese population.
Motor vehicle accidents (MVAs) are common yet un- expected traumatic events in developed countries. In Hong Kong, according to the statistics provided by the Police Public Relation Bureau, 14,014 and 14,714 cases of MVA occurred in Hong Kong in 1998 and 1999, respectively. Besides physical injuries, the psychological consequences of MVA can be chronic, disabling, and catastrophic. A number of studies have suggested the occurrence of psychiatric morbidity in people involved in MVAs.5-10 MVA has also been considered as a significant event that may cause PTSD in Western societies.11 The reported prevalence for PTSD has varied widely from 1%12 to 46%.5
This report focuses on the treatment effect of using EMDR for a person involved in an MVA who has suffered from PTSD after the accident.
Case Report
The case of a 40-year-old man with good past health and no previous contact with the mental health services prior to the present incident of PTSD is reported. During a routine journey in the course of his job, his vehicle crashed with another car leading to the overturning of his vehicle. He and another passenger were trapped inside the car and were rescued by the fire services. The vehicle was a ‘write-off’ after the accident.
During and immediately after the accident, the patient was conscious. He was treated and discharged after attend- ing the accident and emergency department (A&E) for multiple injuries (bruising, haematoma, and abrasion) on the same day of the MVA. He had since attended A&E 4 times within the 14 days after the MVA for persistent neck pain. The physician in A&E recommended 15 days sick leave for the patient after the accident. Medication prescribed for him was mainly for analgesic purposes. This included diclofenac and paracetamol. He was also referred to see a physiotherapist for pain relief. Although he was found to have no significant physical impairment by the A&E physician, who advised him to attend the general out- patient department for the residual pain, he still complained of pain in his neck, right upper limb, and low back 1 month after the MVA.
The patient was referred for clinical psychological services by the A&E physician due to the patient’s excessive worries and sleeping difficulties after the MVA. The patient was undergoing legal litigation related to the MVA through- out the treatment period.
Symptoms of Post-traumatic Stress Disorder
When the patient’s psychological condition was first asses- sed 1 month after the MVA, he satisfied the Diagnostic and Statistical Manual of Mental Disorders – 4th edition (DSM-IV)13 diagnostic criteria for PTSD. The major PTSD symptoms identified included the following:
- Intrusion — the patient reported frequent intrusive thoughts related to the MVA and fear of MVA recurring in the future. He was also disturbed by self-questioning thoughts concerning the reasons, processes, possible preventive measures, and consequences of the MVA.
- Avoidance — since the MVA, the patient avoided talking to others about the accident and playing electronic racing games. He avoided driving as full-time employment and, when he drove, he became cautious of his driving speed, checking his speed more frequently than previously and constantly avoiding exceeding the speed limit.
- Hyperarousal — since the accident, the patient found himself more agitated and scolded his son more frequently. His heightened arousal pattern had also caused initial insomnia and frequent wakening and the sound of a siren would make him fearful and jumpy.
- Functional impairment — the patient’s occupational and social functioning were significantly impaired after the MVA. Prior to the accident, he was socially active and would join the weekly social activities with other drivers. After the accident, his interest decreased and he seldom participated in these activities. Moreover, after the expiration of his sick leave, he was still unable to drive for a few weeks. When he was first seen for the present intervention (1 month after the accident), he could barely work part-time. The patient reported that he could not work on a full time basis because he was too worried and fearful while driving.
Standardised Measurements
The Impact of Event Scale-Revised
The Impact of Event Scale-Revised (IES-R)14 is revised from the Impact of Event Scale,15 which is a short self-reporting measure for capturing the level of symptomatic response to specific traumatic stressors, manifested during the past week. Based on research and the DSM-IV, responses in the realm of intrusion, avoidance, and hyperarousal have been identified as the primary domains of measurement in the IES-R.15 There are 22 items. The patient has to rate how much he or she was distressed or disturbed by each difficulty in the past week on a 5-point scale (0 means “not at all” and 4 means “extremely”).
The severity of symptoms related to PTSD experienced by this patient was measured by the Chinese version of the Impact of Event Scale-Revised. The comparability of the Chinese version of IES-R has been validated by back- translation procedures involving input from the original authors of the IES-R (Wu and Chan, personal communication, 2002).
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS) is a self-reporting rating instrument consisting of 14 items designed to detect symptoms related to anxiety and depres- sion in general medical outpatient populations.16 The patient is instructed to complete the scale to reflect their state in the past week. All 14 items are rated on a 4-point scale, ranging from the absence of a symptom or the presence of positive features (scoring 0) to maximal symptomatology or the absence of positive features (scoring 3).
During the present intervention, this patient’s emotional adjustment was measured by the Chinese version of the HADS.17
Treatment
The EMDR treatment protocol was used for the patient’s treatment.3 Briefly, the patient was asked to identify the picture related to the MVA that he found most disturbing. The most dominant emotions, negative self-statement, and bodily discomfort related to this picture were then examined. After each set of bilateral eye movements (more than 20), the patient was requested to report his level of subjective units of disturbance (SUD) from 0 to 10 (0 represents “neutral and no distress” and 10 represents “the highest possible distress”). After the SUD level reached 0 to 1, positive self-statement was installed until the validity of cognition (VOC) for this statement reached 6 or 7 in a 7- point scale (1 represents “completely false” and 7 means “completely true”). The uncomfortable bodily response was then worked with until the patient felt no particular bodily discomfort when he brought up the originally dis- turbing image. The completion of the above processes may take one to several sessions according to individual response.
After a total of 4 weekly EMDR sessions, the patient’s SUD level decreased from 9 to 2 when he visualised the most disturbing scene of the MVA. Although installation of positive cognition and cleaning out of bodily discomfort associated with the MVA had not been formally started, the validity of positive cognition (“cars are under control and I am now safe to drive on the road”) had spontaneously increased from 1 to 4 as the SUD level decreased. The patient also reported a significant reduction of PTSD symptoms (intrusion, avoidance, and hyperarousal) and felt much less agitated. He also began working full time again. Although he was informed that the treatment process has not yet been completed according to the standard treatment protocol, he requested termination of treatment because of his busy working schedule.
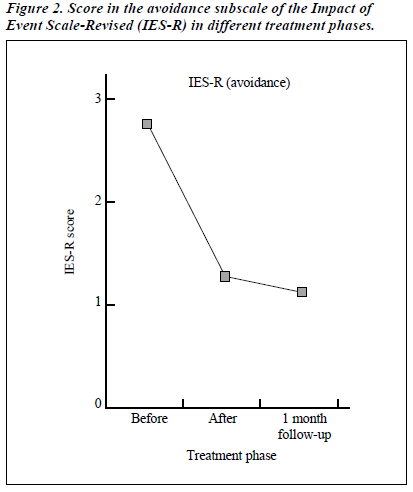
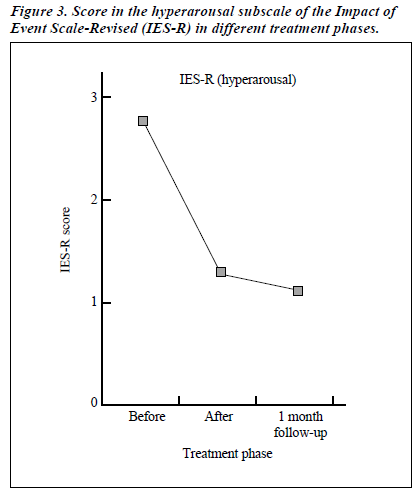
During this EMDR treatment process, the progress of the patients was tapped by his responses in IES-R and HADS. As schematically presented in Figures 1 to 4, improvement was noted in all the subscales of both measures. The improvement was sustained 1 month after the treatment was terminated.
Discussion
This case report provides encouragement for the appli- cation of EMDR in the treatment of PTSD, particularly after MVA. Contrary to expectation, the improvement was substantial and maintained only after desensitisation of disturbances as measured by the SUD level. However, the treatment phase for installation of positive self-statement and ‘cleaning out’ of bodily responses, which are also important elements of EMDR, had not been started. Nevertheless, as noted by Shapiro,3 significant progress could be made after desensitisation has been achieved. The possible reason is summarised as: “by this point in the session the client should have progressed dramatically in the way she feels about the original event. Because of a variety of new insights she may have far surpassed in her own expectations and may now view the event in a much more positive light than originally imagined”.3 This statement is consistent with the treatment response of the present case, as the patient’s VOC spontaneously increased after the desensitisation of disturbances prior to the formal instal- lation phase had begun.
Studies examining the treatment relevance of eye move- ments in EMDR have been conducted. For example, accord- ing to a study comparing 3 forms of EMDR (EMDR with eye movements initiated by tracking a clinician’s finger, EMDR with eye movements engendered by tracking a light bar, and EMDR using fixed visual attention), the eye move- ment conditions were termed “more efficient”.18 However, a recent meta-analysis, which found that EMDR is not more effective than other exposure techniques, suggests that the eye movements are unnecessary.19 Thus, further dismantling studies that examined the use of alternating movements other than eyes would be necessary.
Based on the treatment response of this patient, the examination of specific contribution and relative importance of various EMDR treatment phases is also suggested. If desensitisation of disturbances alone is adequate to produce a sustainable treatment effect, it may be considered as the most essential treatment phase in EMDR. On the other hand, the relative importance of various treatment phases in EMDR may interact with specific factors (level of intrusion, avoidance, hyperarousal, and personal cognitive appraisal style). Exploration of this interactive relationship may help to increase our understanding of the specific treatment needs of each patient.
The treatment response of this specific patient implied that it is possible to apply EMDR for treatment of PTSD among the Chinese population. It also provides encouragement for the cross-cultural generalisation of research evidence on EMDR accumulated in the West.
Similar to most single case reports, the present one is considered only as a limited piece of evidence providing encouragement for the application of EMDR. Well- controlled studies would be needed before the treatment efficacy of EMDR as compared with other treatment options (medication and exposure therapy) for the Chinese population could be confirmed.
References
- Shapiro F. Efficacy of the eye movement desensitisation procedure in the treatment of traumatic memories. J Trauma Stress 1989;2:199-224.
- Shapiro F. Eye movement desensitisation: a new treatment for post-traumatic stress disorder. J Behav Ther Exp Psychiatry 1989;20: 211-217.
- Shapiro F. Eye movement desensitization and reprocessing: basic prin- ciples, protocols, and procedures. New York: The Guilford Press; 1995.
- Chambless DL, Baker MJ, Baucom DH, et al. Update on empirically validated therapies, II. Clin Psychologist 1998;51:3-16.
- Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Gerardi RJ. Psycho- logical morbidity associated with motor vehicle accidents. Behav Res Ther 1994;32:283-290.
- Bryant RA, Harvey AG. Initial posttraumatric stress responses follow- ing motor vehicle accidents. J Trauma Stress 1996;9:223-234.
- Epstein R. Avoidant symptoms cloaking the diagnosis of PTSD in patients with severe accidental injury. J Trauma Stress 1993;4:451-458.
- Hickling EJ, Blanchard EB. Post-traumatic stress disorder and motor accidents. J Anxiety Disord 1992;6:283-304.
- Malt UF, G B. Psychosocial consequences of road accidents. Eur Psychiatry 1993;8:227-228.
- Mayou R, Bryand B, Duthie R. Psychiatric consequences of road traffic accidents. BMJ 1993;307:647-651.
- Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Con- sult Clin Psychol 1992;60:409-418.
- Malt U. The long-term psychiatric consequences of accident injury. Br J Psychiatry 1988;153:610-618.
- American Psychological Association. Diagnostic and statistical manual of mental 4th ed. Washington: American Psychiatric Asso- ciation; 1994.
- Weiss DS, Marmar CR. The Impact of Event Scale-Revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 399-411; 1997.
- Horowitz MJ, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979;41:209-218.
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361-370.
- Leung CM, Ho S, Kan CS, Hung CH, Chen CN. Evaluation of the Chinese version of the Hospital Anxiety and Depression Scale. Int J Psychosom 1993;40:29-34.
- Renfrey G, Spates CR. Eye movement desensitization and reprocess- ing: A partial dismantling procedure. J Behav Ther Exp Psychiatry 1994;25:231-239.
- Davidson PR, Parker CH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol 2001; 69(2):305-316.