Hong Kong J Psychiatry 2002;12(3):19-20
CASE REPORT
R Mahendran
Adjunct Associate Professor R Mahendran MBBS, MMed (Psych), DPM, FAMS, Institute of Mental Health and Woodbridge Hospital, Singapore
Address for correspondence: Adj. Assoc Prof R Mahendran, Institute of Mental Health and Woodbridge Hospital, 10 Buangkok View, Singapore
539747
Tel: (65) 6389 2000, Fax: (65) 6385 1051
Submitted: 1 February 2002; Accepted: 26 March 2002
Abstract
This is a report of a patient with clozapine-induced leucopenia and thrombocytopenia. The latter haematological dysfunction has not been previously reported with clozapine use. The recovery period was also unusually prolonged. Depot injections of zuclopenthixol and flupenthixol, which were given after clozapine was discontinued, could have contributed to the delay in recovery.
Key words: Clozapine, Leucopenia, Thrombocytopenia
Introduction
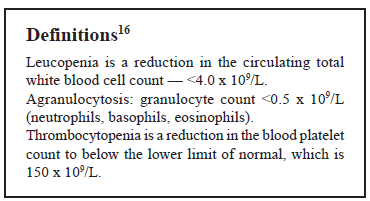
Clozapine is an atypical antipsychotic agent with proven efficacy for the treatment of refractory schizophre- nia. A well known side effect is agranulocytosis, which can occur in 1% to 2% of treated patients.1,2 Other haemato- logical effects include leucopenia, neutropenia, and eosino- philia.3-5 Anaemia, leucocytosis, and increased platelet count have been reported in less than 1% of patients receiving clozapine.6
Product labelling cites thrombocytopenia as occurring ‘very rarely’ with clozapine therapy and a MEDLINE search of the English language literature using the terms ‘thrombo- cytopenia’ and ‘clozapine’ yielded 6 citations between 1966 and 1998. Of these, 1 report related the occurrence of agranulo- cytosis and thrombocytopenia in 2 patients. A second report described lymphocytopenia and thrombocytopenia in a patient treated with risperidone, which continued after switching to clozapine. The third report was of a patient who only had a reduction in platelet count with clozapine and developed epistaxis.
The following is a report of a 41-year-old Chinese man who developed both leucopenia and thrombocytopenia after taking clozapine therapy.
Case Report
This patient was first diagnosed with schizophrenia in 1981 at the age of 24 years. His condition deteriorated thereafter and he has been unemployed since the age of 27 years. He experienced relapses in 1988 and 1990 and, in 1996, was admitted to a psychiatric hospital after a violent attack on neighbours during which he chased them with a chopper.
The patient has been treated with various antipsychotic medications, including trifluoperazine up to 60 mg per day, lithium carbonate 750 mg per day, depot injection flupenthixol 40 mg monthly for approximately 1 year, depot injection fluphenazine decanoate 12.5 mg monthly for 6 months, and depot injection zuclopenthixol 200 mg monthly, increased to 400 mg fortnightly for 1 year, and given with depot flupenthixol 20 mg for 4 months. The patient also received electroconvulsive therapy during his first admission to hospital and again in 1996.
As there was little improvement in his mental state and he experienced extrapyramidal side effects, all oral medica- tions were stopped in April 1997 and he was given risperidone titrated to 6 mg per day. A gradual improvement was noted in that he was less withdrawn and was able to start occupa- tional therapy. However, in October 1997, risperidone had to be discontinued because he suddenly became deluded that the medication was ‘snake poison’ and refused to take it any longer. The patient remained thought disordered, experienced auditory hallucinations, and had bizarre delu- sions. He was preoccupied and socially isolated in the ward but was able to attend to activities of daily living.
In October 1997, the decision was made to give him clozapine. The physical examination at that time was normal and baseline urea, electrolyte levels, liver and thyroid func- tion tests, and complete blood count were within normal limits. The patient was given clozapine 50 mg at night in October 1997. After 17 days, the total white blood cell count fell to 3.2 x 109/L (normal range, 4.5-11.0 x 109/L) and platelets were 122 x 109/L (normal range, 150-450 x 109/L). Clozapine was stopped but the blood monitoring continued. The patient had no fever and no symptoms suggestive of a viral infection or collagen vascular disease. There was no hepatosplenomegaly and investigations revealed normal eryth- rocyte sedimentation rate. Serology for cytomegalovirus, Epstein Barr virus, Parvovirus B, and hepatitis B and C viruses were negative. The prothrombin/prothromboplastin times were normal. Peripheral blood film showed that the majority of red blood cells were well haemoglobinised normocytes.
The findings of a bone marrow and trepine examination in December 1997 showed hypocellular marrow with 3 lin- eages present — granulocytic hypoplasia together with megakaryocytes and normoblastic erythropoiesis were noted, consistent with a drug-induced hypoplasia reaction. The serology for anti-double-stranded DNA antibody and antinuclear antibody were negative.
Twenty days after stopping clozapine, the patient’s mental state deteriorated and he was given depot injections of zuclopenthixol 400 mg and flupenthixol 30 mg in November 1997. This was associated with a sharp fall in white blood cell count to4 x 109/L and platelets to 85 x 109/L. The patient was then given oral haloperidol 3 mg per day at the beginning of December 1997. After 3 weeks, the white blood cell count had increased to 4.7 x 109/L and the platelets to 106 x 109/L. When the depot injections were repeated at the same doses, the white blood cell count decreased to 3.8 x 109/L and the platelets to 90 x 109/L. Following this, a deci- sion was made to stop the depot injections and his condition was maintained with oral haloperidol 5 mg per day. It was only 13 weeks after stopping clozapine that the white blood cell count rose to 4. 8 x 109/L and platelets to 147 x 109/L.
Discussion
This case is unusual because of the occurrence of both leucopenia and thrombocytopenia with clozapine use. In addition, recovery from the bicytopenia was prolonged. Generally, the occurrence of neutropenia and eosinophilia are transient and neutrophil recovery occurs after a mean of 9.3 days. The fall in white blood cell count and platelet levels persisted for almost 13 weeks for this patient — prolonged recovery has not been previously reported. The author suspects the depot injections that were given after clozapine was stopped could have contributed to the persis- tently low white blood cell count and platelet levels. How- ever, there is no documented proof that these compounds could have caused the thrombocytopenia. Furthermore, the patient had been receiving both zuclopenthixol and flupenthixol injections for 4 months without adverse effects. Zuclopenthixol and flupenthixol are also not structurally similar to clozapine.
There is also no indication that the bicytopenia was produced by an immune mediated mechanism as has been suggested in other reports. A repeat bone marrow examina- tion to show recovery after the drug was stopped may be useful, but it was not done as the patient’s haematological findings had returned to normal and the clinicians did not feel that a repeat bone marrow was warranted.
It was recently reported that 3 patients had prolonged granulocyte depression when olanzapine was initiated while experiencing decreased granulocyte levels associated with clozapine use. This is similar to the clinical events for this patient and is a reminder that early institution of other medi- cation for patients with clozapine-induced haematological depression is to be avoided.
References
- Alvir JM, Lieberman JA, Safferman AZ, Schwimmer JL, Schaaf JA. Clozapine induced agranulocytesis incidence and risk factors in the United States. N Engl J Med 1993;329:162-167.
- Alvin JM, Lieberman JA. Agranulocytosis: incidence and risk factors. J Clin Psychiatry 1994;55 (Suppl B):137-138.
- Klimke A, Klieser E. The atypical neuroleptic clozapine — current knowledge and recent clinical aspects. Fortschr Neurol Psychiatric 1995;63(5):173-193.
- Hummer M, Kurz M, Barnas C, Saria A, Fleischhacker WW. Clozapine induced transient white blood count disorders. J Clin Psychiatry 1994:55:429-432.
- Jann MW, Grimsley SR, Gray EC, Chang WH. Pharmacokinetics and pharmacodynamics of clozapine. Clin Pharmacokinetics 1993;24: 161-176.
- McEvoy GK, editor. American Hospital Formulary Services. Author- ity of the Board of Directors of the American Society of Health- System Pharmacists; 1998:1874-1885.
- Idanpaan-Heikkila J, Alhava E, Olkinuora M, Palva IP. Agranulocytosis during treatment with clozapine. Eur J Clin Pharmacol 1977;11:193-198.
- Assion HJ, Kolbinger HM, Rao ML, Laux G. Lymphocytopenia and thrombocytopenia during treatment with risperidone or clozapine. Pharmacopsychiatry 1996;29(6):227-228.
- Durst R, Dovevitch A, Fraenkel Y. Platelet dysfunction associated with clozapine therapy. South Med Journal 1993;86:1170-1172.
- Hummer M, Kurz M, Barnal C, Fleischhacker WW. Transient neutro- penia induced by clozapine. Psychopharmacol Bull 1992;28:287-290.
- Vial T, Proflet C, Pham E, Payen C, Evreux J C. Acute drug-induced agranulocytosis. Therapie 1996;51:508-515.
- Pisciotta AV. Drug-induced agranulocytosis. Peripheral destruction of polymorphonuclear leucocytes and their marrow precursors. Blood Rev 1990;4:226-237.
- Gerson SL, Meltzer H. Mechanisms of clozapine-induced agranulocy- tosis. Drug Saf 1992;7 (Suppl):17-25.
- Lieberman JA, Johns CA, Kane JM, et al. Clozapine induced agranulo- cytosis: non-cross reactivity with other psychotropic drugs. J Clin Psychiatry 1988;49(7):271-227.
- Flynn SW, Altman S, MacEwan GW. Prolongation of clozapine induced granulocytopenia associated with olanzapine. J Clin Psychop- harmacology 1997;17:494-495.
- Dace JV, Lewis SM editor. Practical Haematology International Student. 7th ed. Publisher Churchill Livingstone, London 1991.