Hong Kong J Psychiatry 2002;12(4):14-22
ORIGINAL ARTICLE
RMK Ng, SP Leung
Acknowledgements: We would like to thank all the nurse raters and the nurse trainer, Mr Joe Wong for administering Rehabilitation Evaluation Hall and Baker scales to the study group. We are much indebted to
Dr PC Iu, Dr HK Cheung, and Dr CH Yuen for facilitating us to administer the Rehabilitation Evaluation Hall and Baker scales to patients in the respective adult teams. We would also like to thank our last Hospital Chief Executive, Dr HS Ng, for supporting this hospital-wide research. We would also like to take this opportunity to thank Mr Albert Mak, our ex- Departmental Operation Manager of team 2, who is the pioneer in intro- ducing this Rehabilitation Evaluation Hall and Baker scale to Castle Peak Hospital. Castle Peak Hospital Training Fund sponsored this research.
Dr Roger MK Ng, MBchB, MRCPsych (UK), FHKAM(Psychiatry), Senior Medical Officer, Kowloon Hospital, Kowloon, Hong Kong, China.
Dr SP Leung, MBBS, MRCPsych (UK), FHKAM(Psychiatry), Chief of Service, team 2, Castle Peak Hospital, Hong Kong, China.
Address for correspondence: Dr RMK Ng, Kowloon Hospital, Kowloon, Hong Kong, China.
E-mail: rmkng@netvigator.com
Submitted: 24 June 2002; Accepted: 24 August 2003
Abstract
Objective: To study the nature and severity of disabilities in adult patients admitted to Castle
Peak Hospital in Hong Kong for more than 6 months.
Methods: A sample of 783 patients (606 men and 177 women) was surveyed in a 5-month period from July to November 1999. The Rehabilitation Evaluation Hall and Baker scale, a well-validated observer-rated scale, was applied to the sample. The 46 raters who administered the Rehabilitation Evaluation Hall and Baker scale were trained nurses (‘nurse raters’). Results: Forty four percent of the sample (n = 345) had at least 1 deviant problem, predominantly self-talking behaviour (37.8%) and verbal aggression (19.2%). Female patients were more violent both physically and verbally, and also exhibited more self-talking behaviour compared with males. The patient mix in various types of wards suggests that these wards served their original purposes, as patients with more deviant problems were cared for in the acute and ‘resistant’ wards. Patients staying for more than 6 years exhibited more severe behaviour deficits, suggesting that they were in need of more intensive and novel approaches in the rehabilitation process. Overall, approximately 45% of patients (n = 343) were in the severe handicap range. Conclusions: This study has confirmed that a large proportion of chronic psychiatric inpatients are severely disabled, with a wide range of deviant behaviour and general behaviour deficits. Intensive and novel approaches for rehabilitation would be needed to facilitate their resettlement in the community.
Key words: Inpatients, Chronic disease, Rehabilitation, Psychiatric status rating scales, Hong Kong
Introduction
In Hong Kong, as in the West, chronic mentally disabled patients have been the focus of public concern.1 It has been shown in prospective studies that community care can improve the quality of life of chronic psychiatric patients, in terms of reduction of negative symptoms and expansion of social network.2 However, the cost of re-provision in the community is potentially the same or more expensive than hospital stay.3
For the most difficult-to-place patients, the cost of residential care in the community is clearly higher than in- hospital care.3 Inadequately funded community services will likely lead to homelessness and trans-institutionalisation.4
Reports of scandals associated with care in the community have been prevalent in the West.5 As discussed by Bachrach, de-institutionalisation should have 3 components:6
- release of hospitalised patients into the community
- prevention of subsequent re-admission into hospital
- the provision of adequate alternative psychiatric services in the community.
The distinct lack of the last component was noted in many countries with unsuccessful de-institutionalisation.7 In part, this lack might be due to the paucity of data about hospitalised chronic patients before they were re-settled into the community.
Community care for psychiatric patients has been developing steadily during the past few decades in Hong Kong, but there are many hurdles, one of which is resource constraint.8 As suggested by Mak and Yip, healthcare resources should be planned and provided.8 Before resources can be allocated to reprovision services in the community, the deficits and rehabilitation needs of the patients have to be well understood.
Western data have suggested that both ‘new’ long-stay9 and ‘old’ long-stay patients10 in psychiatric hospitals in the West have persistent, severe psychotic symptoms and residual deficits. In the absence of data about disabilities in the long-stay patients in psychiatric hospitals in Hong Kong, it would be extremely difficult to estimate the extent of residential and rehabilitation facilities required in the community to re-settle these chronic patients.10,11
The objective of this study was to understand the type and extent of disabilities in the chronically hospitalised patients in a psychiatric hospital in Hong Kong. It was hoped that the results would identify the patients’ behavioural problems and assist with planning of rehabilitation services for patients residing in Castle Peak Hospital, and possibly also in other psychiatric institutions in Hong Kong. The second part of the study (discussed in a separate paper) tests the predictive validity of the Rehabilitation Evaluation Hall and Baker (REHAB) scale in predicting the success of discharge into the community.
Methods
Sample and Demographic Data
The study commenced in July 1999 and ended in November 1999. The study subjects were all patients aged 18 to 65 years who had been residing in Castle Peak Hospital for more than 6 months. Exclusion criteria included organic brain syndrome, substance misuse, and mental retardation as the principal diagnosis. All of the sample patients were identified through the database system in the Castle Peak Hospital. Nurse raters collected data on the gender, age, duration of hospitalisation, ward type, and the principal diagnoses according to the ICD-10 criteria.
Assessment Instrument
The REHAB scale12 was selected for this hospital-wide survey. The REHAB scale is used for global assessment of social functioning in chronic psychiatric populations, and has been shown to have good inter-rater and test-retest reliability.13 The scale is composed of 2 item formats, one on deviant behaviour and the other on general behaviour.
The deviant behaviour format screens for the presence and degree of severity of 7 deviant problem areas: incontin- ence, absconding, sexual acts, talking to self, violence, verbal aggression, and self-injury. Each problem can be rated according to the degree of severity, as follows: no or mild problem = 0; moderate problem, target behaviour occurring once in a week = 1; severe problem, target behaviour occur- ring more than once in a week = 2.
The general behaviour format can be divided into 5 factors: social activity, self-care, community skills, speech disturbance, and overall rating. Under each factor, there are several factor items. The 5 factors therefore give rise to 16 factor items. For each factor item, a rating ranging from 0 to 7 can be assigned on a visual analogue scale, using a line with 3 cues below it — 1 at the left, 1 in the middle, and 1 at the right. Under the self-care factor, there are 5 factor items: table manners, washing, dressing, looking after possessions, and prompting. Under the factor of community skills, 2 items are assessed: money use and use of public facilities. Under the speech disturbance factor, there are 2 items: amount of speech and clarity of speech. Under the factor of social activity, there are 6 items: mixing on ward, mixing off ward, spare time, activity, amount of speech, and initiation of speech. Finally, the factor of overall rating allows the rater to give a global clinical impression of the patient.
Two workshops were organised by an experienced nurse trainer, to train 46 nurse raters in 22 wards for this survey exercise. Nurse raters were required to have been working in the participating wards for at least 3 months, and could only rate patients with whom they had been well acquainted for at least 3 months. An inter-rater reliability of 0.91 to 0.95 (pair-wise kappa agreement) [mean, 0.93] was achieved by all nurse raters, in a sub-sample of patients (n = 110) randomly selected from each ward by the random number table method.
Cut-off points of 40 and 65 were used in this survey to identify the distribution of the sample in terms of the rehabilitation potential (0 to 40 = low handicap; 41 to 65 = moderate handicap; 66 to 144 = severe handicap).
Data were analysed using Statistical Package for Social Sciences (SPSS) version 8.0 software. All categorical data were subjected to Chi squared tests or Fisher tests for comparison purpose. All continuous data were subjected to t-tests, or multiple comparison tests, such as analysis of variance (ANOVA) or analysis of covariance (ANOCOVA) models. Bonferroni’s correction was applied when multiple post hoc pair-wise comparisons were required.
Results
Sample Demographics
Of 850 patients identified through the computer database system on 31 May 1999, seven hundred and eightly three patients were available for interview in the study period (July to November 1999). The remainder (n = 67) were discharged from Castle Peak Hospital for community place- ment (n = 56), transferred out for medical reasons (n = 8), or died (n = 3).
The sample of 783 patients represented approximately 50% of the total population in the hospital during the study period, and comprised 606 male patients and 177 female patients. Mean ages according to gender (43.9 years for males and 43.7 years for females) did not differ significantly (t-test, p = 0.82).
The duration of stay was, however, significantly longer for male patients (82.6 months) compared with female patients (69.6 months; t-test, t = 2.04, p = 0.042). As many as 93.7% of the sample suffered from schizophrenia, and 5.1% from bipolar affective disorder; additional diagnoses among the remaining patients included depressive disorders and personality disorders.
Distribution of Deviant Problems
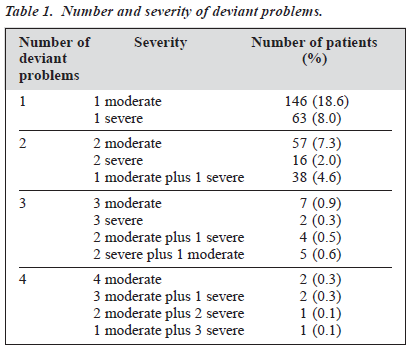
345 patients had at least 1 deviant problem as rated in the total deviant score (i.e. deviant behaviour score of at least 1), representing 44% of the total sample population. As shown in Table 1, most of the patients with deviant problems suffered from one moderate deviant problem (42.3% of all patients with deviant problems).
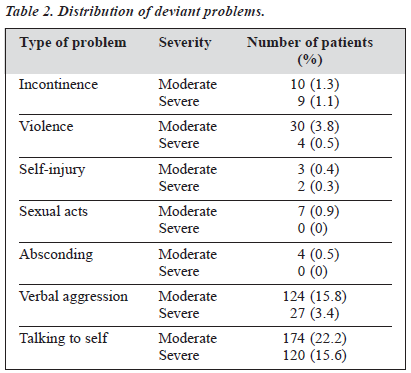
Table 2 shows the distribution of the 7 deviant factors. A substantial proportion of the population (37.8%) exhibited self-talking behaviour at a frequency of once a week or more. Verbal aggression in the form of swearing or scolding others was also common, occurring in 19.2% of the total popula- tion. Two deviant problems, talking to self and verbal aggres- sion, were significantly more common than other deviant problems (Chi squared test, p < 0.005).
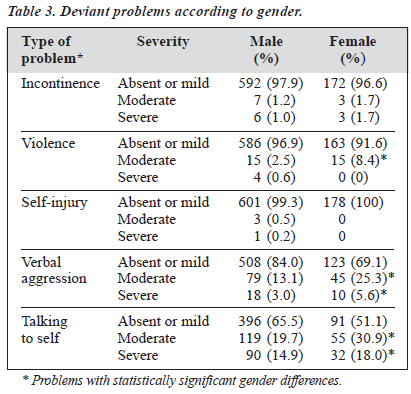
On further analysis of the deviant problems in terms of gender, it is apparent that a greater proportion of female than male patients was physically violent [Fisher exact test, degrees of freedom (df) = 2, p = 0.001] and verbally aggres- sive (Chi squared, df = 3, p < 0.001). Furthermore, a greater proportion of female patients exhibited the abnormal behaviour of talking to self (Chi squared, df = 3, p = 0.003), suggesting that a greater proportion of female patients were psychotic with self-muttering. The p value for statistical significance was set at 0.005 due to there being 10 com- parisons. A breakdown of the deviant problems by gender is shown in Table 3.
A patient was defined as residing in a particular ward if his or her ward status did not change throughout the study period (6 months). The 22 wards were divided into 5 ward types, namely acute wards (n = 67), rehabilitation wards (n = 155), chronic wards (n = 402), forensic wards (n = 81) and treatment-resistant wards (n = 71). Seven patients moved between ward types several times during the assessment and thus categorisation into ward type was not possible.
ANOVA showed that there was a significant between- group difference in terms of age, with planned comparison showing that the resistant-ward patients (mean age, 39.4 years) were significantly younger than the chronic ward patients (mean age, 44.6 years) and the rehabilitation ward patients (mean age, 45.2 years), both comparisons yielding a p value of 0.002 (Bonferroni correction set at 0.003 for multiple comparisons). There was no significant difference in the duration of stay among the 5 groups of patients using one-way ANOVA with Bonferroni correction (p value set at 0.0025)
Table 4 shows the numbers of patients with specified numbers of deviant problems in each ward category. In view of the multiple post hoc pair-wise comparisons required (27 comparisons), Bonferroni correction was made so that only p values of less than 0.002 were regarded as statistically significant.
Comparison of the acute and rehabilitation wards showed that acute wards had a greater proportion of patients with 2 or more deviant problems (Chi squared, t = 22.5, p < 0.001), suggesting that difficult patients tended to remain in acute wards for better management of challenging be- haviour. The difficult nature of the patients in acute wards was further exemplified by the fact that the acute wards and the resistant wards were not significantly different in terms of the proportion of patients with deviant problems (t = 11.7, p = 0.047).
The rehabilitation and forensic wards were similar with regard to patient mix (t = 2.41, p = 0.92; t = 1.23, p = 0.42), but the chronic wards had more patients with 2 or more deviant problems, although the difference was of marginal significance (t = 11.23, p = 0.004). The resistant wards had significantly greater proportions of patients with 1 and 2 or more deviant problems compared with rehabilitation wards (t = 40.2, p < 0.001).
Comparing the chronic wards with the forensic wards, there was no significant difference in the proportion of patients with deviant problems (t = 2.48, t = 0.28). The chronic wards had a significantly lower proportion of patients with 1 or more deviant problems compared with resistant wards (t = 20.2, p < 0.001; t = 23.4, p < 0.001). Again, the forensic wards had a significantly smaller proportion of patients with deviant problems compared with resistant wards (t = 17.1, p < 0.001; t = 13.4, p < 0.001).
In summary, the resistant wards had the highest proportion of patients with deviant problems, while the rehabilitation wards had the lowest proportion of patients with deviant problems. The forensic wards seemed to have a similar case mix as the rehabilitation wards. However, the acute wards seemed to have a backlog of some patients, and thus had a similar proportion of difficult patients as the resistant wards.
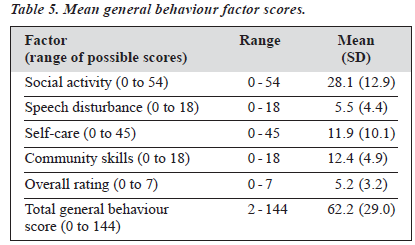
General Behaviour Scores
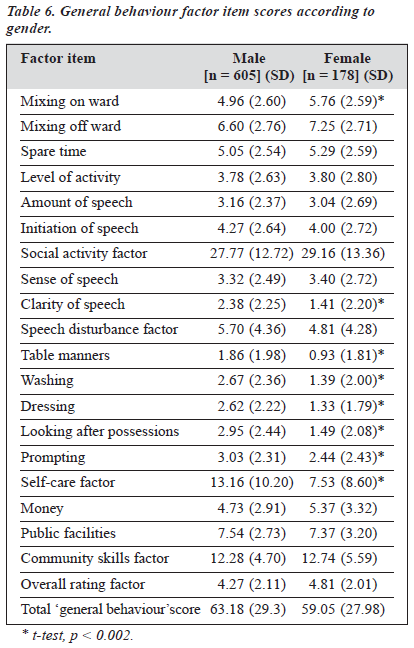
Table 5 shows mean scores for general behaviour format factors and total general behaviour. Overall, mean total general behaviour fell into the range of moderate handicap (41 to 64). Further analysis of the general behaviour scores showed no significant gender differences for the total general behaviour score. However, detailed breakdown of the item and factor scores did reveal differences (Table 6). Again the p value of statistical significance was set at 0.002 in view of a total of 21 comparisons.
On t-test analysis of the factor items, females fared worse than males in terms of mixing on the ward. However, female patients had higher clarity of speech, a finding that might be related to less severe thought disorder. Male patients fared worse than females in self-care in all factor items (table 6) manners, washing, dressing, looking after possessions, and prompting).
There was significant correlation (Spearman) between age and REHAB scores and sub-scores for total social activity (r = 0.135, p < 0.0005), total speech disturbance (r = 0.119, p = 0.001), total self-care (r = 0.079, p = 0.027), total community skills (r = 0.096, p = 0.007), and total general behaviour (r = 0.117, p = 0.001). There was also sig- nificant correlation between the duration of stay and REHAB scores for total social activity (r = 0.188, p < 0.0005), total speech disturbance (r = 0.271, p < 0.0005), total self-care (r = 0.211, p < 0.0005), total community skills (r = 0.57, p < 0.0005), overall rating (r = 0.210, p < 0.0005), and total general behaviour (r = 0.206, p < 0.0005). When partial correlation for age and REHAB scores were carried out with duration of stay controlled, only total social activity was significantly correlated with age (r = 0.10, p = 0.008). When partial correlation for duration of stay and REHAB scores was carried out with age controlled, all correlations re-mained significant (total social activity: 0.20, p < 0.0005; total speech disturbance: 0.27, p < 0.0005; total self-care: 0.20, p < 0.0005; total community skills: 0.20, p < 0.0005; overall rating: 0.23, p < 0.0005; total general behaviour: 0.25, p < 0.0005), suggesting that duration of stay explained most of the age effects on the REHAB scores.
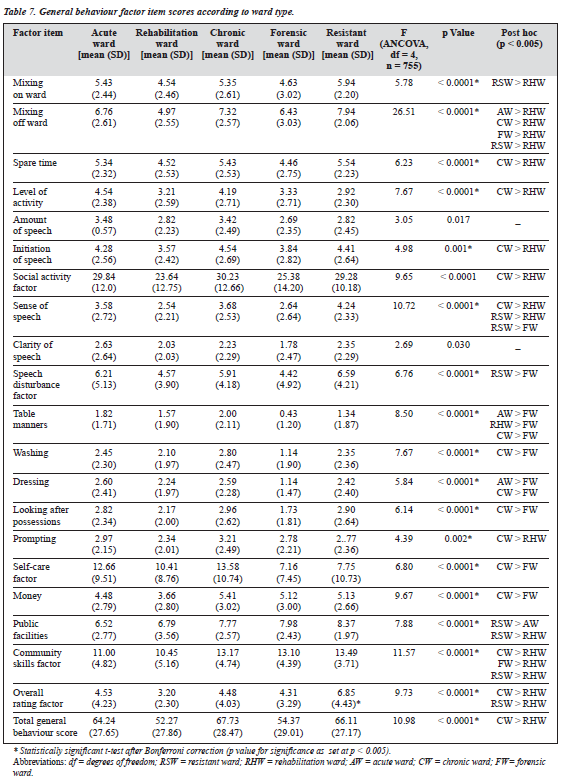
Differences between wards also accounted for some of the REHAB score differences, as shown by analyses per- formed with ANCOVA, with age, gender, and duration of stay as the covariates. Due to multiple comparisons made across different ward types, the p value for significance was adjusted to 0.0025 for comparisons between ward types and to 0.005 for post hoc comparisons. The results showed significant differences in various factor items for patients in different wards (Table 7).
Rehabilitation ward patients were significantly better in mixing off-ward in planned comparisons with the chronic ward, forensic ward, resistant ward and acute ward patients. The opportunity of mixing off-ward in the open setting of the rehabilitation wards might account for the finding. For most of the items under the social activity factor (mixing off ward, level of activity, spare time, and initiation of speech) and for the social activity factor, rehabilitation ward patients fared much better than chronic ward patients (post hoc, p < 0.005). Among the 4 types of wards, the total general behaviour score of rehabilitation wards was highest for rehabilitation wards, with the difference between the rehabilitation and the chronic wards reaching statistical significance (mean difference, 15.46; p < 0.0001). The sense of speech in rehabilitation ward patients was better than in chronic and resistant ward patients, while there was no difference in this factor between rehabilitation ward, forensic ward, and acute ward patients. Forensic patients fared better than resistant ward patients, possibly because the former were detained in forensic wards because of legal requirements.
For the total factor scores from table manners, washing, dressing and total self-care factor scores (table manners plus washing plus dressing plus looking after possessions), forensic ward patients rated significantly better than chronic ward patients (post hoc, p < 0.005). Rehabilitation ward patients fared worse even than forensic patients in terms of table manners. Except for prompting, there were no significant differences between rehabilitation ward patients and chronic ward and resistant ward patients in the items of the self-care factor.
In terms of money use and total community skill factor scores (money plus public facilities), rehabilitation ward patients fared significantly better than the chronic ward patients. On overall rating by the staff, resistant ward and chronic ward patients were judged to be significantly worse than the rehabilitation ward patients. With regard to the total general behaviour score, only chronic ward patients were significantly worse than the rehabilitation ward patients.
New Versus Old Long-stay Patients
Spearman correlation suggested that duration of hos- pitalisation was significantly related to REHAB scores (0.20 to 0.27, p < 0.0005). The sample was divided into 2 groups; those staying less than 6 years as new long-stay patients (n = 481) and those staying more than 6 years (n = 286) as old long-stay patients. This definition was taken from McCreadie to facilitate comparison with the western sample.9
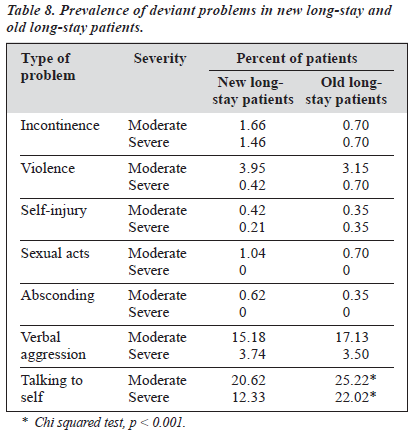
The mean age of the new long-stay patients (42.7 years) was significantly lower than the mean age of old long-stay patients (45.6 years) [t-test, t = 4.15, p < 0.001]. There were also more male patients in the old long-stay group (Chi squared, t = 8.35, p = 0.004). Data on deviant problems in the 2 groups is shown in Table 8.
When the deviant problems were analysed in terms of the nature of the problem, a significantly greater proportion of old long-stay patients exhibited moderate (Chi squared, t = 20.5, p < 0.001).
It is notable that while the mean number of total problems was not significantly different in the new long-stay and old long-stay groups (0.61 and 0.74, respectively), the mean number of severe problems was significantly higher in the old long-stay than in the new long-stay group (0.18 and 0.26, respectively, p < 0.001). There was no significant difference in the mean number of moderate problems in the 2 groups (0.44 and 0.47, respectively, p = 0.56). As a group, old long-stay patients had more intractable deviant problems, especially in talking to self.
Table 9 shows the various factor items of the general behaviour and total general behaviour score in the old and the new long-stay groups. The t-tests demonstrated that the old long-stay patients had significantly poorer scores across all factor/factor item scores except the money item. The lack of difference in the use of money in the 2 groups simply reflected the lack of opportunities in the closed ward patients, regardless of the length of stay, in spending money in the community.
Rehabilitation Potential
The rehabilitation potential of the sample was examined by segregating the subjects into 3 groups, as suggested by Hall and Baker.12 232 patients (29.6%) had high rehabilitation potential for discharge (total general behaviour score £ 40), 208 (26.6%) were in the range of moderate potential (total general behaviour score 41 to 65), while 343 patients (43.8%) had severe handicap with little potential for discharge (total general behaviour score 66 to 144).
Further one-way ANOVA revealed significant differences in the 3 groups of patients in all factor items, all 5 factors, and the total general behaviour score, indicating that the 3 groups were highly different in all aspects of the behaviour assessment in the REHAB scale (all comparisons yielded p < 0.0001). This suggests that the total general behaviour score alone is quite reliable in segregating the patients into different levels of disabilities. Further analysis of the numbers of male and female patients in terms of rehabilitation potential revealed no significant difference (Chi squared, t = 2.39, p = 0.303).
Discussion
This was the first comprehensive survey of chronic psychiatric patients in hospital in Hong Kong, and provides information on the rehabilitation needs of these patients. As community psychiatry gains ground in Hong Kong,14 the data from this study may assist in the provision of a framework for rehabilitation requirements associated with reprovision of services in the community.
Gender and Rehabilitation
It is apparent that female patients were more violent physically and verbally than males in this sample. This is in contrast with studies that have found an association between violence and male gender in the community.15 However, in a large-scale prediction study, Lidz et al found that female inpatients seemed more likely than men to be assaultative.16
Furthermore, female patients usually tended to have a higher chance of discharge to the community, reflecting the general acceptance of female patients back into the role of housewife after psychotic breakdown.17
This is supported by our finding that female patients also appeared to be more psychotic, as manifested in the higher proportion of female patients with deviant behaviour of talking to self. Female patients who stayed for longer than 6 months might be a biased sample of difficult patients. Nevertheless, this highlights the need for comprehensive risk assessment of female inpatients before community reprovision.
On the other hand, male patients had more impaired psychosocial functioning, as reflected in the more severe handicap in self-care skills. This may suggest that male schizophrenic patients had more prominent negative symptoms, which might be related to earlier onset of the illness,17,18 more frequent occurrence of brain abnormalities, and poorer premorbid functioning.19,20,21 Another possible explanation was the longer length of stay in hospital, leading to demoralisation and institutionalisation.22 Training in self-care and community living skills may be beneficial in this regard.23
Ward Nature and Rehabilitation
There were significant differences in the various areas of functioning across different types of wards. Resistant ward and acute ward patients appeared to be the most psychotic, as suggested by the presence of deviant problems in the form of self-talk and verbal violence. The treatment-resistant nature of the psychosis suggests that clozapine24 and cognitive-behavioural treatment of psychosis25 might be particularly valuable in improving their global functioning. The need for more effective treatment is all the more pressing in the resistant ward patients as these were the youngest and had relatively intact self-care and community skills.
The forensic patients had relatively intact life skills with a mean general behaviour score of 54.4, and compared favourably with the rehabilitation ward patients. This relatively good level of functioning may be explained by improvement in life skills through the rehabilitation training of the forensic rehabilitation unit (community re- integration unit). In the present study, the good performance of forensic patients in the area of self-care and social skills could not be attributed to shorter length of stay because there was no significant difference in length of stay across the 5 groups.
A possible explanation is the relatively shorter duration of psychosis for the forensic group, as offending usually starts at an early age.26 It has been argued that there is a critical period of 3 years in the history of psychosis, during which there is rapid deterioration of psychosocial functioning, and after which functioning will remain more or less static.27
Also, younger patients tend to have better social and self- care skills.
New and Old Long-stay Patients: Do They Have Similar Needs?
Previous studies in the UK have suggested that old long- stay patients have severe disabilities that need to be adequately addressed before reprovision in the community.10
A recent study has suggested that poor global functioning and severe psychopathology predict homelessness 3 months after discharge.28 The homeless patients were frequently sent to prison for petty offences arising out of poverty or psychotic symptoms.4 In this survey, old long-stay patients had sig- nificantly more severe deficits in self-care, community and social activity skills.
The Team for the Assessment of Psychiatric Services (TAPS) project in the UK showed that the patients reprovided upon closure of the Friern and Claybury Hospitals showed an improvement in domestic skills and community skills due to increased opportunities to practice the relevant skills.29
Furthermore, Wing argued for the importance of the asylum and protective functions of mental hospitals in the care of these severely impaired patients, emphasising the importance of reprovision of similar asylum and protective functions in community facilities before resettling such old long-stay patients in the community.30
Success in reprovision depends critically on adequate resources for community rehabilitation.31 The TAPS project demonstrated that community care was not cheaper than hospital care and claimed that funding derived from hospital closure should be ‘ring-fenced’ for community care for psychiatric patients.3
Patients staying for less than 6 years in hospital demon- strated better life skills, as reflected in better performance for all factors of ‘general behaviour’ in the REHAB scale. Patients with greater illness severity have greater difficulty achieving resettlement in the community, leading to pro- longed hospitalisation. It is worth noting that, since the establishment of general psychiatric units in regional hos- pitals, chronic patients with higher functioning have been selected and transferred to these new units.
This ‘creaming off ’ process may partly explain the significant correlation between duration of hospitalisation and severity of the REHAB scores. This argument is sup- ported by the fact that the current profile of REHAB scale was similar to the Claybury profile conducted in 1989, which documented a creaming off process, leading to an increasingly ‘hard core’ of remaining patients.32 A further reason for this difference in performance may be the effect of institutionalisation, in that patients undergoing prolonged stay in hospital might develop social poverty syndrome mimicking negative symptoms.33
Based on discriminant function analysis, Hall and Baker found that 4 measures (social activity, community skills, self-care, and total general behaviour scores) correctly classified 77% of patients in either long-stay ward or day hospital.12 Total general behaviour alone could correctly classify 75% of patients. Total deviant behaviour was not useful in this respect. Furthermore, the best discrimination cut-off score for total general behaviour was 40; this score correctly classified 82% day patients and 69% of long-stay patients. A total general behaviour score of over 65 was classified as the disturbing group.
In the current study, it was noted that around 30% of the sample had REHAB scores below 40 and that these patients were concentrated in the rehabilitation wards. Although a REHAB score of below 40 is used as a cut-off score for high discharge potential, evidence has shown that placement decisions should not be based on scores alone.34 Instead, many patients are in need of flexible and intensive rehabilitation before discharge to the community is feasible. In fact, many patients might have special problems not listed in the deviant problem section of the REHAB scale. These problems may include fire risks, refusal to leave hospital, and drinking problems.
Limitations
The major limitation of this study is that only one objective scale, REHAB, was administered to the whole sample. This shed light on the global functioning of the sample population without data on other dimensions, such as psychopathology, quality of life, special problems, and subjective satisfaction. These indicators provide important data for determining the suitability of the patients for resettlement in the community.
Conclusions
This was the first large-scale survey of the disabilities of inpatients with a length of stay greater than 6 months in Castle Peak Hospital. Female patients appeared to be more psychotic while male counterparts had more disabilities in self-care and community functioning. The old long-stay patients were more impaired in psychosocial functioning, suggesting that they require a specific level of care in all aspects of psychosocial functioning if reprovision in the community is to be implemented. For rehabilitation planning in hospital, self-care training will be the first priority in all chronic wards while use of atypical antipsychotics should be considered for the resistant ward patients and those patients with more than 6 months of stay in acute wards.
References
- Carpenter J. Rising to the challenge: meeting the needs of people with severe and long-term mental illness. HK J Mental Health 1992;21: 81-90.
- Leff J. Outcome for long-stay non-demented patients. In: Leff J, editor. Care in the community: illusion or reality? Chichester: Wiley & Sons; 1997:69-92.
- Beecham J, Hallam A, Knapp M, Baines M, Fenyo A, Asbury M. Costing care in hospital and in the community. In: Leff J, editor. Care in the community: illusion or reality? Chichester: Wiley & Sons; 1997:93-108.
- Lamb HR, Shaner R. When there are almost no state hospital beds left. Hosp Community Psychiatry 1984;44:973-976.
- Thornicroft G, Bebbington P. Deinstitutionalisation – from hospital closure to service development. Br J Psychiatry 1989;155:739-753.
- Bachrach, L. A conceptual approach to deinstitutionalization. Hosp Community Psychiatry 1979;37:118-119.
- Bachrach L. Some reflections from abroad. Hosp Community Psychiatry 1982;40:573-574.
- Mak KY, Yip KS. The importance of an effective psychiatric community care service for chronic mental patients in Hong Kong. HK J Mental Health 1997;26:28-35.
- McCreadie RG, McCannell E. The Scottish survey of new chronics: five-year follow-up. Br J Psychiatry 1989;155:348-351.
- McCreadie RG, Stewart M, Robertson L, Dingwall JM. The Scottish survey of old long-stay in-patients. Br J Psychiatry 1991;158:398-402.
- Kendall RE. The future of Britain’s mental hospitals. BMJ 1989; 299:1237-1238.
- Baker B, Hall R. Part 2: technical information: validity. In: Baker B, Hall R, editors. User manual for rehabilitation evaluation. 3rd impression. Aberdeen: VINE Publishing Ltd; 1988:119-121.
- Carson J, Coupar A, Gill J, Titman P. The inter-rater reliability of Hall and Baker’s REHAB scale: a cross-validation study. Br J Clin Psychol 1988;27:277-278.
- Mak KY. Psychiatric rehabilitation in the 21st century: a personal view. Hong Kong J Psychiatry 2000;10:22-24.
- Mullen P. Violence and mental disorder. Br J Hosp Med 1988;40: 460-463.
- Lidz C, Mulvey E, Gardner W. The accuracy of prediction of violence to others. JAMA 1993;269:1007-1011.
- Johnstone E. Schizophrenia. In: Johnstone EC, Freeman CPL, Zealley AK, editors. Companion to psychiatric studies. Edinburgh: Churchill Livingstone; 1998:369-398.
- Hafner H, Riecher A, Maurer K, Loffler W, Munk-Jorgensen P, Stromgren E. How does gender influence age at first hospitalization for schizophrenia? Psychol Med 1989;19:903-918.
- WHO. Schizophrenia. An international follow-up study. Chichester: Wiley; 1979:194-199.
- Angermeyer MC, Kuhn L, Goldstein JM. Gender and the course of schizophrenia: differences in treated outcomes. Schizophr Bull 1990;16:293-308.
- Jablensky A, Sartorius N, Ernberg G, et al. Schizophrenia: manifesta- tions, incidence and course in different cultures. A World Health Organization ten-country study. Psychol Med Monogr Suppl 1992; 20:1-97.
- Carpenter WT, Kirkpatrick B. The heterogeneity of the long-term course of schizophrenia. Schizophr Bull 1988;14:645-659.
- Test MA. Training in community living. In: Liberman RP, editor. Handbook of psychiatric rehabilitation. Boston: Allyn and Bacon; 1992:153-170.
- Meltzer HY. Atypical antipsychotic drug therapy for treatment-resistant In: Hirsch SR, Weinberger DR, editors. Schizophrenia. Oxford: Blackwell; 1995:485-502.
- Garety PA, Fowler D, Kuipers E. Cognitive-behavioral therapy for medication-resistant psychotic symptoms. Schizophr Bull 2000;26: 73-86.
- Taylor P. Schizophrenia and risk of violence. In Johnstone EC, Freeman CPL, Zealley AK, Companion to psychiatric studies. 2nd ed. Edinburgh: Churchill Livingstone; 1998:163-183.
- Birchwood M, McGorry P, Jackson H. Early intervention in schizo- phrenia. Br J Psychiatry 1999;170:2-5.
- Olfson M, Mechanic D, Hansell S, Boyer CA, Walkup J. Prediction of homelessness within 3 months of discharge among inpatients with schizophrenia. Psychiatr Serv 1999;50:667-663.
- Leff J, Trieman N. Long-stay patients discharged from psychiatric hospitals. Social and clinical outcomes after five years in the community. The TAPS Project 46. Br J Psychiatry 2000;176:217-223.
- Wing J. The function of asylum. Br J Psychiatry 1990;157:822-827.
- Leff J, Knapp M, Carrier J, Trieman N. Beyond the asylum. Reprovision for psychiatric hospitals: recommendations from TAPS/PSSRU research findings. Health Serv J 1995;105:28-30.
- Carson J, Shaw L, Willis W. Which patients first: a study from the closure of a large psychiatric hospital. Health Trends 1989;21:117-120.
- Wing JK, Brown G. Institutionalism and schizophrenia. Cambridge: Cambridge University Press; 1970:125-165.
- Conning AM, Brownlow JM. Determining suitability of placement for long-stay psychiatric inpatients. Hosp Community Psychiatry 1992;43:709-712.