Hong Kong J Psychiatry 2003;13:34-38
Case Report
YK Miao
Abstract
Mania sometimes occurs in association with an organic condition in the brain. A 29-year-old housewife with secondary mania related to multiple sclerosis is described. The case highlights the importance of considering organic causes in treating patients with mania, especially when there are unexplained neurological findings and cognitive dysfunction. The case also illustrates the usefulness of magnetic resonance imaging for investigating organic causes of secondary mania and psychosis.
Key words: Bipolar disorder, Case report, Diagnosis, Magnetic resonance imaging, Multiple sclerosis
Acknowledgements: Thanks to Dr Tsoi Tak Hon, Consultant, Department of Medicine, Pamela Youde Nethersole Eastern Hospital; Dr Dunn Lai Wah, Eva, Consultant, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital; and Dr Yeung Sau Heung, Medical Officer, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital.
Dr Yin King Miao, MBBS, MRCPsych(UK), FHKAM(Psychiatry), Senior Medical Officer, Department of Psychiatry Pamela Youde Nethersole Eastern Hospital, Hong Kong, China.
Address for correspondence: Dr Yin King Miao, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, 3rd Lok Man Road, Chai Wan, Hong Kong, China.
Submitted: 12 October 2002; Accepted: 21 February 2003
Mania sometimes occurs in association with an organic condition. The diagnosis of a hypomanic episode according to DSM-IV requires a distinct period of persistently elevated, expansive, or irritable mood, lasting at least 4 days, with at least 3 associated symptoms, such as inflated self-esteem, decreased need for sleep, talkativeness, racing thoughts, distractibility, increased goal-directed activity or psycho- motor agitation, and excessive involvement in pleasurable activities.
The diagnosis of a hypomanic episode must be dis- tinguished from a mood disorder due to a general medical condition. Very often, the florid psychopathology can ob- scure subtle neurological/physical signs and symptoms, and make the diagnosis of the underlying organic conditions difficult.
Multiple sclerosis (MS) is a particularly devastating disease of the central nervous system (CNS); a patient’s presenting symptoms and the temporal evolution of the clinical findings may suggest the correct diagnosis. In relapsing-remitting MS — the type present in 80% of patients — symptoms and signs typically evolve over a period of several days, stabilise, and then often improve, spontaneously or with treatment, within weeks. Relapsing- remitting MS has a peak age of onset of 20 to 40 years and has a female predominance of approximately 2:1. This type of MS typically starts with sensory disturbances, uni- lateral optic neuritis, diplopia, limb weakness, clumsiness, gait apraxia, and neurogenic bladder and bowel symptoms. Twenty percent of affected patients have primary progressive MS, while others may develop persistent neurological signs after relapse and the disease may progress between relapses (secondary progressive MS).
Prominent cortical signs (aphasia, apraxia, recurrent seizures, visual field loss, and early dementia) and extrapyra- midal phenomena (chorea and rigidity) only rarely dominate the clinical picture. Eventually, cognitive impairment, de- pression, emotional lability, dysarthria, dysphagia, vertigo, progressive quadriparesis, and other CNS manifestations become troublesome.
The diagnosis is based on established clinical, and when necessary, laboratory criteria. The most widely used diag- nostic criteria are Poser’s criteria.1 Very recently, a new criterion developed by McDonald has been found to en- able earlier diagnosis in a group of patients with one demyelinating syndrome.2 It may become widely used in the near future.
On magnetic resonance imaging (MRI), findings of multifocal lesions of various ages, especially those involving the periventricular white matter, brain stem, cerebellum, and the spinal cord white matter, support the clinical impression. The presence of gadolinium-enhancing lesions on MRI indicates current sites of presumed inflammatory demye- lination (active lesions). Cerebrospinal fluid (CSF) analysis often shows increased intrathecal synthesis of immuno- globulins of restricted specificity, oligoclonal bands may be present, or the synthesis of immunogobulin G (IgG) may be increased. Physiological evidence of subclinical dys- function of optic nerves and spinal cord (changes in visual evoked responses and somatosensory evoked potentials) may further support the diagnosis.
A case of a 29-year-old married woman with secondary hypomanic features associated with multiple sclerosis (MS) is presented, along with a review of the subject. This is the first reported case of mania associated with multiple sclerosis in a Chinese woman, and highlights the impor- tance of considering organic causes when treating patients with mania.
Case Report
Ms C was first referred to our unit in December 2000 with a 1-month history of increased irritability, elated mood, over- talkativeness, and disturbing behaviour. She had no family or personal psychiatric history. Her premorbid personality was described as even-tempered and hard working. She was neither a smoker nor a drinker and had never abused illicit drugs. She had no past forensic record.
Ms C denied any disturbances in sleep and appetite, buying sprees, or promiscuity. During the initial interview, she appeared to be overfriendly, but without grandiose thoughts. There were no psychotic symptoms. Complete blood count, renal and liver function tests, venereal disease research laboratory results, and electroencephalogram were all normal. She was diagnosed as suffering from hypomania and prescribed low-dose haloperidol, 1.5 mg daily.
In January 2001, she was admitted to the United Christian Hospital for urinary incontinence and limb weakness. She was discharged after 2 days with no definitive diagnosis. In the following month, her limb weakness and incontinence resolved. Around this time, she was arrested twice for shop- lifting. She denied any intent to steal, claiming that she simply forgot to pay. She was charged and received a fine.
In March 2001, she was admitted to Queen Elizabeth Hospital again for recurring bilateral limb weakness. She was ambulatory and had no incontinence. Neurological examination and computerised tomography revealed no abnormality.
After discharge, relatives reported Ms C to be rather dull and unresponsive. Her volition was also poor, with forget- fulness. However, she denied any low mood or loss of interest. A mini-mental state examination (MMSE) revealed a score of 28/30; she lost 2 marks from the serial 7’s test. There was some impairment in attention and concentration. Clinically, she was suspected to be in the depressive phase of bipolar disorder. She was prescribed fluoxetine.
Three months later, in June of 2001, she was admitted to our ward via casualty for increased irritability, decreased sleep, over-talkativeness, displaying disinhibited behaviour of urinating in public places, and running away from home. According to relatives, from April to June, she had on and off episodes of unsteady gait. Family noted that she was capable in most activities of daily living, but they found her mood and personality changes difficult to cope with and very upsetting. Her husband decided to divorce her.
During admission, Ms C looked to be perplexed. From time to time, she would suddenly dash out from the room and rush into the nurses’ station. Her sleep and appetite was preserved. No incontinence was noted.
Mental state examination revealed Ms C to be rather over-friendly and carefree. Her affect was not elated. She was oriented to time, place, and persons. She could give her own history in good chronological order. Her speech was largely relevant and coherent, and no confabulation was noted. There were no psychotic symptoms. Her short- term memory was intact. However, her performance in attention and concentration tasks and verbal fluency tests were unsatisfactory. She had no insight and had no understanding of why she was brought to hospital.
Physical examination showed that she was afebrile, and vital signs were normal. Neurological examination revealed bilateral upgoing plantar. There was no loss of muscle power. Her gait was normal.
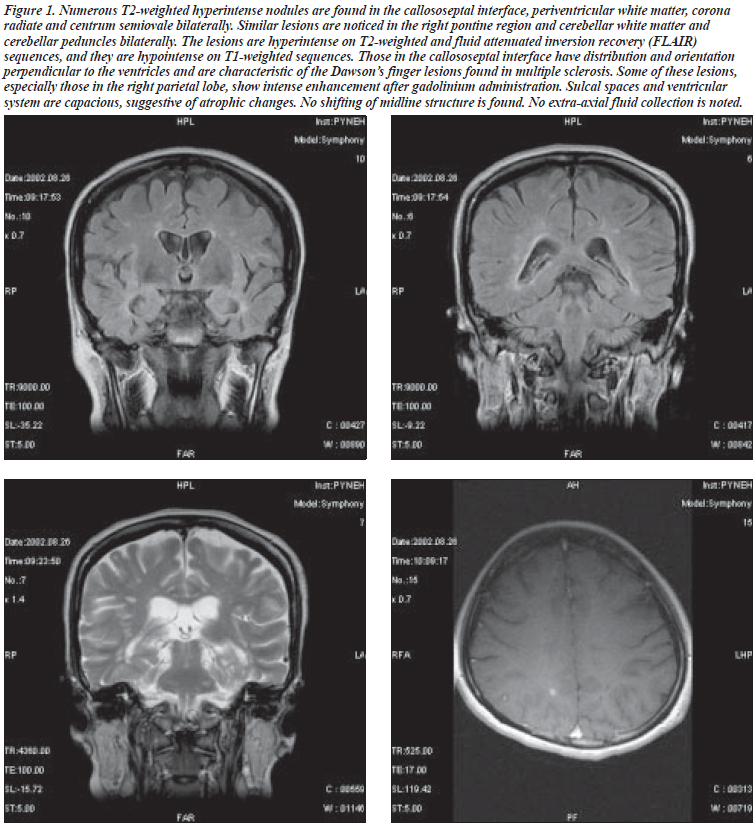
MRI revealed multiple T2 brightenings in the supra- tentorial white matter in the calloso-septal interface, the right and the left middle cerebellar peduncles and at the left side of the pons, with some lesions at the supratentorial white matter. Also, there were 3 enhanced lesions: 1 in the right frontal, 1 in the left temporo-parietal, and the other in the posterior portion of the left temporal lobe; they were all suggestive of active lesions of MS (Figure 1).
The patient was then transferred to a medical ward. CSF examination showed positive oligoclonal band and elevated IgG of 18.6 g/dL (normal range, 6.94 to 16.18). Visual and somatosensory evoked potential was performed with prolongation of latencies noted in both. The presence of relapsing and remitting type multiple sclerosis was estab- lished by recurrent episodes of neurological dysfunction, typical MRI findings, positive oligoclonal band and the electrophysical studies. The diagnosis of organic mood disorder, secondary to multiple sclerosis, was made.
Discussion
Secondary mania has multiple aetiologies,3 some related to intracerebral conditions (such as trauma, tumours, cerebro- vascular disorders, epilepsy, normal pressure hydrocephalus, multiple sclerosis, idiopathic basal ganglia calcification, CNS systemic lupus erythematosis, dialysis dementia, tuberous sclerosis, and meningitis), and some to systemic diseases. Reported infectious causes have included human immunodeficiency virus, neurosyphilis, influenza, enteric fever, Q fever, and cholera, tetanus, and typhoid immuni- sation. Drug-induced causes have been widely described, with implicated agents including antidepressants, broncho- dilators, cannabis, coffee, phenylpropanolamine, cortico- steroids, and phenytoin. Metabolic disturbances, such as Cushing’s disease, hyperthyroidism, haemodialysis, and uraemia have also been reported.
The prevalence of multiple sclerosis varies considerably around the world.4 The prevalence is highest in northern Europe, southern Australia, and the central part of North America. Therefore, in Caucasians, MS is one of the most common neurological diseases, especially in women. However, the prevalence in Asian countries is low, and considered less than 5 cases per 100,000 persons. A study reported by Lau et al found the prevalence of Chinese MS sufferers was about 0.77 per 10,000 persons,5 with a high female-to-male ratio of 9.6:1. Most patients (72%) had
relapse-remitting type MS, a figure similar to Caucasian populations. The Chinese MS patients also had a high rate of spinal cord involvement (66%) and a low presence of CSF oligoclonal banding (40%). Shiu et al also noted that in Chinese MS, transverse myelitis was more common than optic neuritis (66.7% versus 25.9%).6
Although psychiatric and cognitive abnormalities are common manifestations of the disease, depressive symptoms (irritability, poor concentration, low mood, and anxiety) have been the more commonly described in MS. The latter has a lifetime prevalence in MS of around 50%. Euphoria if present, tended to occur in those with advanced disease with cognitive impairment, and was more closely related to MRI lesion load.7
Garland suggested that while there was a correlation between chronic depressive symptoms and both progressive disability and lack of social support in MS, acute major depressive and manic episodes may be psychiatric manifestations of demyelinating lesions and may be the initial presenting symptoms in MS.8 Fisk, in a survey of a hospital-based psychiatric service utilisation and morbidity in MS, found that bipolar disorder and depression were twice as prevalent in hospitalised MS patients as in the general population of hospital users.9 Also, the estimated frequency of suicide attempts was at least 3 times greater in the MS patients.
According to Pine, inpatients with MS presenting to a psychiatric hospital were more likely to have manic psychosis than the inpatient population as a whole, and may or may not present with neurological symptoms typical of MS.10 Schiffer found that there were 10 patients with both MS and bipolar disorder from Monroe County, New York,11 while the epidemiological data indicated that the expected number would be 5.4. A systemic psychiatric evaluation in 100 consecutive patients attending an MS clinic found that 42% had a lifetime history of depression and 13% fulfilled criteria for manic-depressive disorder, indicating the exist- ence of an association between mania and MS.12
There are a number of reports on mania associated with MS. These include a 15-year-old girl,13 2 patients with rapid cycling bipolar disorder and multiple sclerosis,14 and a woman with psychotic onset of MS.15 Casanova described an 81-year-old woman with a 30-year history of bipolar disorder with an autopsy finding of widespread peri- ventricular demyelinated plaques characteristic of MS.16 Natale described a case of MS with manic psychosis at the onset.17
The 29-year-old woman was suffering from manic psychosis for 15 years and had a 5-year history of ataxia, speech troubles, and urine incontinence, with a subsequent diagnosis of MS. Salmaggi reported on a patient with MS and bipolar disorder, with parallel fluctuations of psychiatric and neurological symptoms.18 Therefore, while MS patients account for only a small population of all psychiatric admissions, clinicians should consider the diagnosis of MS in patients exhibiting symptoms in tandem with unexplained neurological findings.
Our patient had no personal or family history of affective disorder. For the 6 months after the onset of her psychiatric problems, she had waxing and waning neurological complaints before the definitive diagnosis of multiple sclerosis. The presence of neurological signs and cognitive dysfunctions (poor performance in concentration and verbal fluency tests) suggested an organic cause for her mania.
Das, comparing patients with organic mania and bipolar disease, found that the organic manics were more often irritable and more likely to make threats, have delusions, and show cognitive dysfunctions.19 Other features suggestive of organicity included absence of personal and family history of major affective disorder, older or atypical age of onset, and the occurrence of manic symptoms during febrile illness.
Advanced brain imaging has not yet been applied systematically to affective illness.20 Mania has been related to focal, right limbic areas and orbitofrontal, temporobasal and temporopolar lesions.21-25 Kellner suggested that diffuse or multifocal white matter lesions could be related to mood disorder.14 Feinstein assessed 10 patients with psychosis and MS and 10 MS patients without psychosis.26 All underwent MRI and it was found that the psychotic group tended to have a higher total lesion score, particularly around the periventricular areas. Our patient had active lesions in the right frontal, left tempore-parietal, and posterior left temporal areas. It was uncertain whether they were strategically located lesions that caused the mania in this case of MS.
Conclusion
There are various causes and mechanisms associated with secondary mania. Clinicians should have a high index of suspicion in those cases with negative personal and family history, late or atypical age of onset, and with unexplained neurological findings. Adequate neuroimaging such as MRI should be considered for investigating organicity.
Mania in MS is a diagnostic challenge. In most cases, neurological symptoms have preceded the onset of psychosis. There may be an aetiological association between the pathological processes of MS and psychosis, and such association warrants further research on the neurobiological basis of psychosis and affective disorder.
References
- Poser CM, Scheinberg L et al. New diagnostic criteria for multiple sclerosis. Ann Neurol 1983;13:227-231.
- McDonald WI, Compston A, Edan G, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol 2001;50:121-127.
- Krauthammer C, Klerman GL. Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry 1978;35:1333-1339.
- Noseworthy, JH. Medical progress: multiple sclerosis. N Engl J Med 2000;343:938-952.
- Lau KK, Wong LKS, Li LSW, Chan YW, Li HL, Wong V. Epidemiological study of multiple sclerosis in Hong Kong Chinese: questionnaire survey. Hong Kong Med J 2002;8:77-80.
- Shiu KL, Tsoi TH, Cheung CM, Au Yeung M, Hon FK. First demyelinating syndrome and risk of progression to multiple sclerosis in Chinese patients. Eur J Neurol 2002;9(Suppl 2):222.
- Ron MA, Logsdail SJ. Psychiatric morbidity in multiple sclerosis: a clinical and MRI study. Psychol Med 1989;19:887-895.
- Garland EJ. Multiple sclerosis and affective disorders. Can J Psychiatry 1991;36:112-117.
- Fisk JD. Hospital-based psychiatric service utilization and morbidity in multiple sclerosis. Can J Neurol Sci 1998;25:230-235.
- Pine DS. Patients with multiple sclerosis presenting to psychiatric hospitals. J Clin Psychiatry 1995;56:295-306.
- Schiffer RB. Association between bipolar affective disorder and multiple sclerosis. Am J Psychiatry 1986;143:94-95.
- Joffe RT. Mood disorder and multiple sclerosis. Arch Neurol 1987;44:376-378.
- Heila H. Case study: mania associated with multiple sclerosis. J Am Acad Child Adolesc Psychiatry 1995;34:1591-1595.
- Kellner CH. Rapid cycling bipolar disorder and multiple sclerosis. Am J Psychiatry 1984;141:112-113.
- Monaco F. Psychotic onset of multiple sclerosis. Ital J Neurol Sci 1980;1:270-280.
- Casanova MF. Multiple sclerosis and bipolar disorder: a case report with autopsy findings. J Neuropsychiatry Clin Neurosci 1996;8:206-208.
- Natale E. Description of a case of multiple sclerosis with psychotic disorders at the onset. [In Italian]. Riv Neurol 1986;56:271-275.
- Salmaggi A. Parallel fluctuations of psychiatric and neurological symptoms in a patient with multiple sclerosis and bipolar affective disorder. Ital J Neurol Sci 1995;16:551-553.
- Das A. Organic manic syndrome: causative factors, phenomenology and immediate outcome. J Affect Disord 1993;27:147-153.
- Swayze VW, Andreasen NC, Alliger RJ, Ehrhardt JC, Yuh WTC. Structural brain abnormalities in bipolar affective disorder. Arch Gen Psychiatry 1990;47:1054-1059.
- Robinson RG, Boston JD, Starkstein SE, Price TR. Comparison of mania and depression after brain injury: causal factors. Am J Psychiatry 1988;145:172-178.
- Rundell JR, Wise MG. Causes of organic mood disorder. J Neuropsychiatr 1989;1:398-400.
- Starkstein SE, Mayberg HS, Berthier ML, et al. Mania after brain injury: neuroradiological and metabolic findings. Ann Neurol 1990;27:652-659.
- Starkstein SE, Fedoroff P, Berthier ML, Robinson RG. Manic-depressive and pure manic states after brain lesions. Biol Psychiatry 1991;29: 149-158.
- Jorge RE, Robinson RG, Starkstein SE, Arndt SV, Forrester AW, Geisler
- FH. Secondary mania following traumatic brain injury. Am J Psychiatry 1993;150:916-921.
- Feinstein A. Psychotic illness in multiple sclerosis: a clinical and magnetic resonance imaging study. Br J Psychiatry 1992;680-685.