Hong Kong J Psychiatry 2003;13(3):23-30
ORIGINAL ARTICLE
Abstract
Objective: The aim of this study was to explore the phenomenon of severe hoarding in Hong Kong.
Patients and Methods: Patients with hoarding problems were recruited through referrals to an outreach psychiatric team by community welfare agencies. A home visit was made to every patient. Semi-structured interview on hoarding, mental state examination, and psychometric assessment were conducted.
Results: Thirty patients were assessed. Thirteen (43%) were men and 17 (57%) were women. The mean age was 54.9 years.The mean age of onset of hoarding was 43.87 years. The mean duration of hoarding was 11.07 years. Nine categories of hoarded items were identified. More than half of the patients had more than 90% of their floor space covered by hoarded items. Patients appeared to underestimate the severity of hoarding and minimise the extent of disturbance to others. Twenty four patients were diagnosed with formal psychiatric disorders, with schizophrenia being the most common diagnosis (n = 14). Fourteen patients were already known to the psychiatric services when assessed. Of the 16 who were not previously known, 6 had no mental illness.
Conclusions: Severe hoarding was mainly found among the lower socioeconomic class. Its onset was mostly in middle age and such behaviour had persisted for a long time. While the majority of hoarders had psychiatric problems, others did not. Every hoarder should receive a formal psychiatric assessment. The relationship between hoarding and various psychiatric illnesses warrants further investigation.
Key words: Behaviour, Cluttering
Dr Siu Ning Chiu, MBChB, MRCPsych, FHKCPsych, FHKAM (Psych), Senior Medical Officer, Kwai Chung Hospital, Kwai Chung, Hong Kong. Mr Heung Chuen Chong, MSocSci (Clinical Psychology), Clinical Psychologist, Kwai Chung Hospital, Kwai Chung, Hong Kong.
Ms Sharon Pui Fan Lau, Nursing Officer, Kwai Chung Hospital, Kwai Chung, Hong Kong.
Address for correspondence: Dr Chiu Siu Ning, Senior Medical Officer, Kwai Chung Hospital, 3-15, Lai King Hill Road, Kwai Chung, Hong Kong.
E-mail: snchiupsy@so-net.com.hk
Submitted: 1 June 2003; Accepted: 22 September 2003
Introduction
Hoarding is defined as the “acquisition of and failure to dis- card possessions that appear to be useless or of limited value”.1 Although collecting is a normal human instinct, hoarding is different from normal collecting and, in some cases, is regarded as a pathological condition. The items hoarders collect are usually useless and they are placed in a non-systematic manner. Instead of enjoying the collection, hoarders may feel ashamed of the behaviour but still feel compelled to hoard and have difficulty discarding the hoarded items. This results in their living spaces being so seriously cluttered as to preclude normal daily activities and causes significant distress or impairment in functioning for the hoarder.
As a psychiatric symptom, hoarding is most commonly found in obsessive compulsive disorder (OCD). The prevalence rate in this disorder ranges from approximately 18% to 30%.2,3 In the Yale-Brown Obsessive Compulsive Scale (Y-BOCS), ‘hoarding/saving obsession’ is one of the rating items.4 The earlier Leyton Obsessional Inventory also has several items related to hoarding.5 In the Fourth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), hoarding is one of the diagnostic features for obsessive compulsive disorder.6 The relationship between hoarding and OCD is clear.
Other authors have reported hoarding in various psychiatric disorders. In a sample of 133 patients with dementia in a Taipei psychogeriatric ward, 30 patients (22.6%) showed hoarding behaviour.7 However, the prevalence of hoarding was much lower (1.9%) in another study in elderly Japanese people.8 Hoarding can also be found in other psychiatric disorders such as organic psychiatric disorders, psychotic disorders, anorexia nervosa, Prader-Willi syndrome, frontal lobe syndrome following head injury, and hippocampal dysfunction.9-14 Yet hoarding behaviour as a symptom in these disorders is limited to case reports in the literature, so the prevalence rate is not known.
The question of whether hoarding behaviour is a familial trait is inconclusive. Frost and Gross reported that 84% of women and 57% of men who were hoarders described their first-degree relatives as hoarders as well.1 This figure is difficult to interpret, however, since the rate of hoarding among first-degree relatives of non-hoarders is unknown. Adams postulated that childhood material deprivation might be one of the predisposing causes for hoarding.15 In this study, Adams found that 28% of hoarders reported some kind of material deprivation early in life, and the hoarders believed that this explained their behaviour.
In studies of items hoarded, Frost and Gross, in a sample of 32 college students showing hoarding behaviour, reported more than 100 different types of items.1 These included clothing (81%), magazines (50%), bags (43%), books (40%), school papers (37%), and cards and letters (31%). Although hoarding is usually connected with inanimate objects, there were reports of people hoarding animals. For example, Thomas described an elderly man with Alzheimer’s disease who kept more than 80 cats at home.16
Some authors believe that not all hoarders are mentally ill. For example, Hogstel divided hoarding into ‘adaptive’ and ‘maladaptive’ types.17 Adaptive hoarding is commonly found among elderly people and is like a hobby for a lonely person. Other authors have tried to explain hoarding behaviour within a psychological context. Furby used the term ‘sentimental saving’ to emphasise the emotional attachment a hoarder has for a possession.18 Fromm suggested that hoarders derived a sense of security from collecting and saving things.19 Frost et al proposed that hoarders regarded the possessions as extensions of themselves, and would use every means to protect the possessions from being disposed of.20 Melamed et al hypothesised that the age of the hoarded items might have a special meaning for elderly people, in that the items might symbolise relationships with others who were no longer living, and that collecting might express denial of ageing.21 Adopting a cognitive-behavioural model, Frost and Hartl regarded hoarding as a multifaceted problem, including information processing deficits, problems in forming emo- tional attachments, behavioural avoidance, and erroneous beliefs about the nature of possessions.22
Management of hoarding is difficult. Studies have focused on 3 aspects of management: pharmacological, social, and cognitive-behavioural. For patients with a psychiatric illness, treatment of the underlying disorder sometimes improves the hoarding behaviour. No particular symptom-specific drug shows superior effectiveness. On the contrary, a case report describing the addition of risperidone to clozapine showed worsening of the hoarding behaviour in a 36-year-old Chinese woman with hebephrenic schizophrenia.23
Social management of hoarding often poses great difficulty to community workers. Hoarders are often reluctant to have their items disposed of. Furious reaction has often been reported when law-enforcement officers carried out their duty of compulsory removal of hoarded items. Frost and Gross conceptualised hoarding as an avoidance behaviour tied to ‘indecisiveness’, so hoarders find it hard to choose which item to discard, even when forced to do so.1
There are only a handful of successful reports of psychological intervention for hoarders. The use of psycho- dynamic psychotherapy has been reported to be useful for patients with obsessive compulsive personality disorder.24 Hartl and Frost derived a cognitive-behavioural treatment approach for successfully treating a 53-year-old woman with compulsive hoarding.25 Hogstel suggested some behavioural strategies by which the severity of the hoarding behaviour could be reduced without jeopardising the relationship between the worker and the hoarder. However, the strategies were applied to elderly people without psychiatric illnesses.17
To date, no single intervention is promising. In line with this, Vostanis and Dean considered that a move to more protected accommodation was the only practical measure that led to a degree of improvement.26 Greenberg stated that only legal pressure could force hoarders to limit their behaviour.27
In Hong Kong, there has been no local study of hoarding behaviour. However, psychiatrists and their colleagues, especially those who perform regular outreach home visits, are often astonished by the scene at a hoarder’s house. In Kwai Chung Hospital (KCH), 1 of the 2 psychiatric hospitals in Hong Kong, the community psychiatric team (CPT) often receives referrals from the public about residents who fill their houses with useless items, and psychiatric problems are suspected. In fact, mental health service staff are usually the last person to contact the hoarders. Before that, the Housing Department and the Social Welfare Department may have received multiple complaints from the hoarder’s family and neighbours. It is believed that those referred to the psychiatric services represent only the tip of the iceberg, and the problem is far more common in the community than previously believed.
In this study, the hoarding problem in Hong Kong is explored in an attempt to answer the following questions:
- What are the characteristics of the hoarders?
- What are the psychiatric problems associated with hoarding?
- Is there any psychological meaning to the hoarders in the items they hoard, if they are not psychiatrically ill?
- Is there any clinical implication for the management of hoarding with the findings obtained?
Patients and Methods
Patients
Community organisations that have a high chance of contacting hoarders were invited to make referrals to the CPT of KCH. These organisations included various family service centres of the Social Welfare Department, Grassroot Organization Development Project of Caritas, The Society for Community Organization, Yang Memorial Methodist Social Service, Hong Kong Christian Social Service, and the community nursing services.
Letters were written to invite referrals. In the letter, the objective of the study and the definition of clinical hoarding were introduced. After obtaining the consent of the hoarder, an outreach home visit would be made by a psychiatrist, a clinical psychologist, and a community psychiatric nurse. The hoarder had to reside within the catchment area of the community psychiatric team (covering a population of approximately 1.5 million). The hoarder had to fulfil the following inclusion criteria of clinical hoarding:
- he/she acquired and failed to discard a large number of possessions that appeared to be useless or of limited value
- his/her living space was sufficiently cluttered because of hoarding, such that activities for which those spaces were designed are precluded
- he/she faced complaints or hygiene problems as a result of the hoarding behaviour.
Patients were excluded from the study if they collected items for daily consumption or use, for selling, and/or the collected items were for collections such as stamps, shells, or music.
Patients and Methods
Patients were assessed with a semi-structured interview comprising the following components. A questionnaire on demographic data, which captured important personal data such as sex, age, educational level, marital status, occupation, income, size of residence, and number and relationships of persons living together, was given.
A questionnaire on the nature, extent, and possible associated factors of hoarding was administered. This questionnaire attempted to examine the phenomenon of hoarding, and included questions about the onset and the duration of hoarding, items hoarded and their sources, perceived benefits and meaning, problems encountered, management of hoarded items, subjective rating of severity of hoarding, subjective rating of self-distress, perceived level of disturbance to others, family history of hoarding, and experience of childhood material deprivation. The question- naire also included an estimated percentage of floor area being occupied by the hoarded items, as judged by the investigators.
The Mental State Examination was used for psychiatric diagnosis based on the Tenth Edition of the International Classification of Diseases (ICD-10).28 Further interviews and other necessary investigations were arranged as necessary.
The Mini-mental State Examination, Cantonese version (MMSE-C) is a rater-rated instrument for evaluation of cognitive impairment, consisting of 2 parts. The first part assesses the patient’s orientation, memory, and attention. The second part tests the patient’s ability to name objects, follow verbal and written commands, write a sentence, and copy a complex polygon. The maximum score is 30. Based on the original MMSE,29 Chiu et al translated a Cantonese version and performed a validation study.30 In Chiu et al’s study of Chinese patients, the MMSE-C yielded a high sensitivity (97.5%) and specificity (97.3%) when using a cut-off score of 19/20. Thus a score of lower than 20 is suggestive of cognitive impairment. However, caution should be exercised when interpreting the results for patients with low literacy level.
The Global Assessment of Functioning Scale (GAFS) is a rater-rated instrument to assess the patient’s overall level of functioning. It is a modified version of the Global Assessment Scale originally developed by Spitzer et al.31
After assessing the psychological, social, and occupational functioning, the rater gives an overall impression of the patient’s level of functioning on an analogue-numerical scale ranging from 1 to 100. The scale represents a hypothetical continuum of mental illness. Every 10 points signifies a different level of functioning. A healthy person with superior functioning in a wide range of activities will have a score between 91 and 100. The scale has been incorporated into the DSM-IV as one of the multi-axial assessments. When used as a psychiatric tool for assessment, the instruction in DSM-IV is that “impairment in functioning due to physical and environment limitations should not be included”. However, for the purposes of this study, the impairment of functioning due to cluttering of residential space is also included when using the GAFS.
The Test of Nonverbal Intelligence Third Edition (TONI- 3) is a non-verbal, language-free measure of cognitive ability. It is culturally deduced and has minimal motor requirements. It estimates intellectual competence by evaluating an individual’s skill at solving novel abstract/figural problems. The TONI-3 has been found to be a highly reliable, internally consistent test with minimal content sampling error. It has an averaged coefficient a of 0.93 for both forms of the test. The test-retest (with 1 week time lapse) coefficients are greater than 0.90 for both forms of the test at all ages tested. The TONI-3 has been correlated positively with the results of 3 intelligence tests: the Comprehensive Test of Nonverbal Intelligence, the Wechsler Intelligence Scale for Children Third Edition, and the Wechsler Adult Intelligence Scale Revised.
Results
Thirty five referrals were received from January 2000 to October 2001. Outreach home visits were made to all the referred people. Two declined to be interviewed. Three did not meet the criteria of clinical hoarding because they sold the things collected solely to make a living. Thirty people were assessed.
Demographics
Thirteen hoarders (43%) were men and 17 (57%) were women. The age of the hoarders ranged from 21 to 78 years, with a mean of 54.90 years (standard deviation [SD], 15.72 years), a medium of 51 years, and a mode of 40 years. Sixteen hoarders (53%) were younger than 60 years and 14 (47%) were aged 60 years or older.
The number of siblings (including the hoarders) ranged from 1 to 12, with a mean of 5.33 (SD, 3.15). Nine hoarders (30%) were the eldest (including those who were only children), 6 (20%) were the second eldest sibling, and 5 (16.7%) were third eldest.
Fifteen hoarders (50.0%) were never married, 4 (13.3%) were married, 3 were separated (10,0%), 1 was divorced (3.3%), and 7 were widowed (23.3%). Fifteen hoarders (50%) lived alone, while the rest lived with family members (including parents, brothers, or spouse and children, but not sisters).
The number of years of formal education ranged from 0 to 14, with a mean of 5.88 years (SD, 4.40 years). The majority (22 of 30; 73.3%) depended on Social Security Allowance while others lived on personal savings or family support. Thirteen hoarders (43.3%) were unemployed at the time of the interview, 12 (40.0%) were retired, 3 (10.0%) attended a sheltered workshop, 1 (3.3%) was a part-time causal worker, and 1 (3.3%) was a hawker. The amount of regular monthly income (including Social Security Allowance) ranged from nothing to HK$7000, with a mean of HK$1742 ± HK$1598, and a medium of HK$1500.
The size of residence ranged from 80 to 1000 square feet, with a mean of 265 square feet (SD, 197 square feet), and a median and a mode of 200 square feet. The number of years they had been in residence ranged from 0.42 years to 43.00 years, with a mean of 12.79 ± 11.07 years, a median of 10 years, and a mode of 4 years.
Nature and Extent of Hoarding
The mean age of onset of hoarding was 43.87 years (SD, 19.05 years). The age of onset ranged from 8 years to 76 years, with a median of 41 years and a mode of 60 years (n = 5). There were 8 people (26.7%) living alone at the time when the hoarding began. Seven hoarders (23.3%) were living with parents and 6 (20%) with parents and siblings. The duration of hoarding ranged from a few months to 46 years. The mean duration was 11.07 years (SD, 10.20 years), with a medium of 9 years, and a mode of 2 years, 8 years, 15 years (n = 3 for each mode).
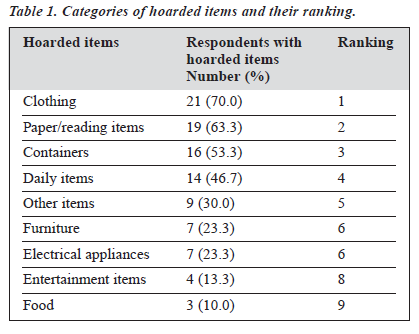
More than 78 common items were hoarded, as observed by examiners and reported by respondents, forming 9 main
categories. Respondents usually hoarded more than 1 category of items. Table 1 lists the categories, their respective rank in terms of frequency, and the corresponding number of respondents having hoarded each category.
Hoarders obtained the items from more than 1 source. The most common source was rubbish bins or garbage collection points in the vicinity (n = 20; 66.7%). Other sources included “offers by others”(n = 18; 60.0%), “out of own purchase” (n = 14; 46.7%), “from workplace” (n = 4; 13.3%), and “asking others to give them” (n = 3; 10.0%).
The estimated percentage of floor area occupied by the hoarded items ranged from 20% to 100%, with a mean of 77.67% (SD, 27.56%), a median of 95%, and a mode of 100% (n = 8) [Figures 1 and 2]. More than half of the hoarders had more than 90% of their floor space covered by hoarded items. Eight hoarders had 100% of their floor area filled up, such that they had to either live outside the flat, in the public area, or to walk over the items (mostly waste papers and magazines) at home.
The majority of the respondents (83.3%) claimed that they hoarded for material gain, while 26.7% said that psychological or emotional gain was most important. Among the 8 hoarders who reported the latter, 5 failed to give an
elaborate account. The questionnaire was so designed that once the hoarders reported psychological or emotional gain being more important, they would be invited to give a more detailed account in an open question format. For the remaining 3 hoarders, 2 felt that possession of excess items meant that they could help the poor in case they were asked, and that they felt they still contributed to society despite their old age. One hoarder gave the following explanation: she was a young lady whose mother died before the onset of hoarding. Her father started to bring different ladies home, which she regarded as an insult to her deceased mother. She started to hoard so that the home would become a mess, but soon her hoarding behaviour grew out of control.
Extent and Nature of Perceived Distress
When respondents were asked how often the hoarding caused them distress, 18 hoarders (60.0%) reported rarely, 6 (20.0%) reported sometimes, and 6 (20.0%) reported often. When they were asked how often hoarding caused distress to their family, 14 respondents (46.7%) reported rarely, 7 (23.3%) reported sometimes, and 8 (26.7%) reported often. One respondent did not answer this question. Meanwhile, interpersonal conflicts were the most commonly reported cause of distress. Others included difficulty in finding items, embarrassment, poor hygiene, and legal involvement such as being charged with obstructing the walkway.
The most reported persons making complaints about the hoarders were neighbours, parents, children, and the staff of the Housing Department. Twenty one hoarders (70.0%) reported that they simply ignored these complaints. Only 5 hoarders (16.7%) said that they would comply as much as possible. Other reactions included “became angry and retorted” (10.0%) and “would not allow others to throw away or tidy up” (6.7%). Meanwhile, when hoarders were asked what they would do if there were compulsory removal of the hoarded items by the authorities, they gave a wide range of responses. The most common response was “feel angry and will retort ”. Others included: “hoard new items”, “report to the police and sue”, “will not allow and will fight”, “accept reluctantly”, “let them do it”, “ask for money as compensation”, “move away from the residence”, “attempt to locate and bring back the removed items”, “feel relieved”, and “feel at a loss”.
Perceived Severity of Hoarding Behaviour
When respondents were asked to rate the severity of their hoarding behaviour on a 1 to 10 Likert scale, with 1 indicating least severe and 10 most severe, 10 respondents gave a rating of 1 and 5 respondents gave a rating of 10. Such results suggest that they considered their hoarding behaviour either as “not severe at all” or “very severe”.
Nine of 21 respondents claimed to have attempted to stop hoarding. Analysis revealed that 3 of these respondents did not have mental illness while 6 had mental illness. In other words, the majority of those with mental illness (n = 18; 75%) did not attempt to stop hoarding. Meanwhile, 11 respondents reported regular management of the hoarded items, as follows: sorting (n = 10), washing the items (n = 4), selling the items (n = 2), spraying insecticide (n = 1), and taking them to their home village in China (n = 1).
Associated Factors
Only 2 respondents (6.7%) reported a positive family history of hoarding. Meanwhile, 21 hoarders (70%) reported experience of childhood material deprivation, and 14 (46.7%) believed that such past experience was related to their hoarding behaviour.
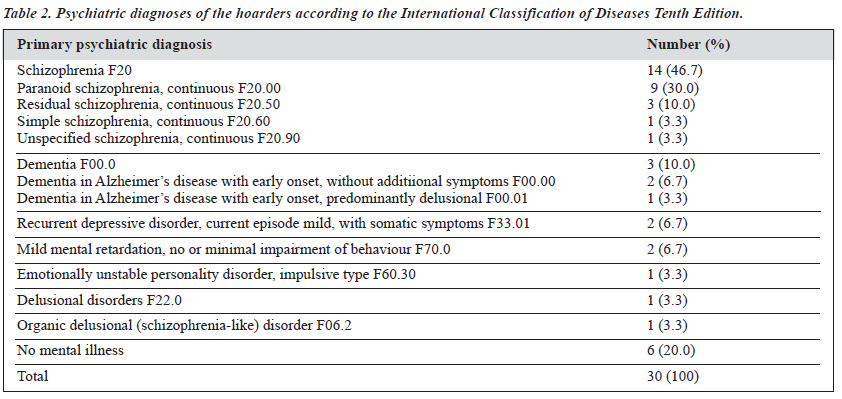
Twenty four hoarders were diagnosed with formal psychiatric disorders while 6 had no mental illness. For those patients who were psychiatrically ill, schizophrenia was the most common diagnosis, accounting for 46.7% of the group. One respondent was diagnosed with residual schizophrenia as the primary diagnosis and obsessive compulsive disorder as the secondary diagnosis. It should be noted that 14 of the 30 respondents were already known to the psychiatric services when assessed. For those who were not previously known to the psychiatric services (n = 16), 6 had no mental illness, 4 had schizophrenia, 3 had dementia, 2 had mild grade mental retardation, and 1 had recurrent depressive disorder. It should be noted that admission to a psychiatric hospital was arranged if necessary, and relevant investigations and intervention were done. Table 2 lists the psychiatric diagnosis of the patients.
The MMSE-C score ranged from 15/30 to 30/30, with a mean of 25/30 (SD, 4.28). Two respondents scored less than 20/30, indicating cognitive impairment. The GAFS ranged from 20 to 100, with a mean of 66.73 (SD, 20.05). Eight respondents scored 50 or below, indicating serious symptoms or serious impairment in social, occupational, or school func- tioning. The TONI-3 scores ranged from 65 to 115, with a mean of 81.43 (SD, 10.68). Two respondents scored below 70, suggesting mental deficiency. Overall, the results of these measures were consistent with the psychiatric diagnoses.
Discussion
The respondents of this study were characterised by the presentation of severe hoarding that caught the attention of
concerned parties such as social service agencies, welfare organisations, housing departments, and community psychiatric nurses. The severity of the hoarding behaviour was confirmed by the study findings. For example, the median duration of hoarding was 9 years, and the median percentage of degree of cluttering was 95%. This study is unique in that most other studies involved hoarders with non-clinical behaviour and of lesser severity.
Analysis of the background of the respondents indicated that the majority were of middle age, had minimal education, were either unemployed or retired, relied on public assistance, did not have a confiding relationship, lived alone, and resided in small public housing units. Such a com- position is largely a reflection of the lower socioeconomic status of the citizens residing in the catchment area of the CPT of KCH, and the way respondents were recruited. Caution should therefore be exercised when interpreting the findings as the sample characteristics may colour the results and affect the generalisability.
In this group, the most salient finding was that 24 of 30 respondents (80%) had a psychiatric diagnosis. The most common psychiatric disorder was schizophrenia. This finding raised questions of the role of severe hoarding in the overall symptom architecture of some psychiatric disorders. Does severe hoarding represent an erroneous belief (“I feel secure only when every inch of my flat was occupied and no aliens could land themselves on my flat”), a disturbed perception (“I can still see plenty of room in my flat although I have to climb over the piles to get to my bed”), disorganised behaviours (“I have managed my household well by placing items here and there and everywhere”), an aftermath of longstanding self-neglect due to depression (“I don’t care”), or a compulsive ritual with reinforcers (for example, intermittent material rewards, or attention from authorities)? How does hoarding relate to and interact with other cardinal psychiatric symptoms? Is hoarding a prodromal pheno- menon or a consequence of certain psychiatric disorders?
These are a few of the many questions that future research may address. Meanwhile, we believe that hoarding is not uncommon in psychotic disorders. The need of hoarders for psychiatric consultation (preferably with on-site assessment) appears clear as 10 of the 24 psychiatrically ill respondents were not previously receiving psychiatric care.
Interestingly, contrary to previous observation, severe hoarding in this group was not strongly associated with OCD. Only 1 respondent was diagnosed with OCD as a secondary comorbidity to the primary diagnosis of residual schizophrenia. Several explanations appear plausible. First, patients with OCD do not hoard to a severe degree to avoid attracting attention. Second, patients with OCD who did hoard severely also developed other rituals (for example, cleaning and checking rituals) that prevent complaints or hygienic problems. Third, as community psychiatric nurses were one of the referring agents, the sample might be biased toward those with severe mental illness such as schizo- phrenia, and the incidence of hoarding among patients with OCD was under-reported. Fourth, there may be qualitative and quantitative differences among different psychiatric disorders, and hoarding in OCD is less conspicuous com- pared with its manifestation in schizophrenia.
Why do people hoard if they are not mentally ill? The findings of this study do not allow us to postulate a cohesive and comprehensive psychological model. When looking at the 6 hoarders with no psychiatric illness, they hoarded items of the same nature as did their mentally ill counterparts. Four of them considered that material gain was of primary importance and only 2 respondents treasured the psycho- logical gain. These 2 hoarders shared some common characteristics: they were older than 70 years, widowed, lived alone in a public housing unit, and were dependent on social security. Since they failed to elaborate on the psychological or emotional gain, we attempted to elicit their life story and found striking similarities in their backgrounds, which could be portrayed as follows. An elderly lady experienced material deprivation in her childhood, strove to earn a living by working hard as a domestic maid or garment factory worker, developed the habit of saving ‘non-worthless’ items, sent or brought these items regularly to her poor relatives in her home village in China out of piety or charity, lived alone after her husband’s death or retirement, continued to lead a primitive yet self-contained and contented life, was well-received in her area, was offered plenty of ‘useless’ items by her neighbours, was suspected by some health care workers to have dementia, became infuriated when her collection was at stake, and actively hoarded possessions during her retirement. Apparently, different motivating forces were in operation, interweaving with one another as her environment and experience evolved.
With regard to the age of onset of hoarding behaviour, the finding of middle age-onset contrasted with that reported by Frost and Gross (childhood and adolescence onset)1 and by Greenberg (in the third decade of life).27 More than one- third of respondents in this study started hoarding after the age of 60 years and, among this group, 3 (27.2%) had no psychiatric diagnosis. Taking into account that 60 years is the formal retiring age, it may mean loss of acquaintances, emotional attachment to workmates, and the working environment, which could trigger ‘adaptive hoarding’ or ‘sentimental saving’.
One surprising finding in this group was the persistence of hoarding behaviour over time. There were several possible factors perpetuating the problem. First, hoarders tended to underestimate the severity of their hoarding. Second, they tended to underestimate the distress caused by hoarding to themselves and others. Third, the perceived material gain may be a very strong perpetuating force for the behaviour to continue.
Consistent with the study of Frost and Gross,1 clothing and paper products dominated the list of hoarded items. Detailed examination revealed that all the rare and bizarre items were collected by patients with schizophrenia. For instance, one patient collected lubricant floating on the sea in small bottles, while another brought home wasted wheel tyres from the dumping ground. Both of these hoarders failed to give a reasonable account of their acts.
Findings from this study may help the management of hoarding behaviour. First, as the majority of the sample was diagnosed with psychiatric disorders, we advocate that every hoarder should receive a formal psychiatric assessment. In particular, hoarders with a rather absurd collection and an early onset of hoarding, who made no attempt to stop hoarding, should receive early attention.
Second, a non-confrontational approach may engender less resistance from the hoarders. As reported above, 70% of responders would ignore any complaints against themselves and more than half of the respondents said that they would “feel anger and retort” if they had their items thrown away against their will. Their reaction may be understandable, given that they did not perceive hoarding as distressing or severe. Eleven respondents even reported that they were actively engaged in regular management of the hoarded items. A non-confrontational approach that seeks to understand the reasons for hoarding, the ways of managing the hoarded items, and the impact on other aspects of life may elicit more cooperation than one demanding immediate removal of the items with a complaining attitude.
It should be noted that 2 respondents had been allocated new housing units, probably as a last resort by the concerned authority against their hoarding behaviour. Yet, after moving to the new residence, they started to hoard again. Thus, simply changing the place of abode may not address the issue of severe hoarding.
The relatively small sample size precluded the applica- tion of advanced statistics. Yet several trends may warrant the attention of interested researchers. For example, the percentage of cluttering among those without psychiatric diagnosis tended to be larger (mean, 87.50%) than those with a psychiatric diagnosis (mean, 71.79%). Female respondents (n = 12; 71%) tended to hoard ‘containers’ more than their male counterparts (n = 4; 31%). Those without a psychiatric diagnosis (n = 2; 34%) tended to ask others for ‘worthless’ items more than their counterparts with a psychiatric diagnosis (n = 1; 4%). Those with a history of childhood material deprivation (n = 12; 57%) tended to report no interpersonal conflicts due to hoarding more than their counterparts with no history of childhood material deprivation (n = 1; 13%). Those without a history of childhood material deprivation (n = 4; 57%) tended to report more trouble to the family due to hoarding than their counterparts with a history of childhood material deprivation (n = 3; 14%).
This exploratory study sought to enrich the understanding of hoarding, but the findings raised more questions than they answered. The fundamental problem is a lack of operational criteria of ‘pathological’ hoarding. The working criteria used here were modified from the definition of hoarding derived by Frost and Gross,1 so could be arbitrary. The sensitivity and accuracy of the measurement in the degree of cluttering should also be refined as many hoarders hoard beyond their residing flat and the volume of their collection cannot be fully captured by a 2-dimensional measure. This study was also limited by its cross-sectional nature, with heavy reliance on the respondents’ own account. Further research could adopt a longitudinal design with naturalistic observation, with informants offering collateral information, targeted at a larger sample.
Conclusion
With the present sample, severe hoarding was found in the lower socioeconomic group of the middle- to old-aged population who lived in public housing units. Its onset was mostly in middle age and such behaviour had persisted for a long time without being noticed. While some hoarders had psychiatric problems, others, especially some elderly hoarders, were mentally well. The relationship between hoarding and various psychiatric illnesses requires further investigation. We advocate that every hoarder should receive a formal psychiatric assessment.
Acknowledgement
We would like to thank the following community agencies for their kindness in referring hoarders to us for this study: Family Service Centers of the Social Welfare Department, Grassroot Organization Development Project of Caritas, The Society for Community Organization, Yang Memorial Methodist Social Service, Hong Kong Christian Social Service and the Community Psychiatric Nursing Service. We would also like to express our gratitude to the hoarders in this study, who allowed us to make home visits and, in some instances, allowed us to take pictures of their homes.
References
- Frost RO, Gross RC. The hoarding of possessions. Behav Res Ther 1993;31:367-381.
- 2. Rasmussen SA, Eisen JL. Clinical features and phenomenology of obsessive compulsive disorder. Psychiatric Annals 1989;19:67-73.
- Frost RO, Krause M, Steketee G. Hoarding and obsessive compulsive symptoms. Behav Mod 1996;20:116-132.
- Goodman WK, Rasmussen SA, Price LH, et al. Yale-Brown Obsessive Compulsive Scale I. Development, use and reliability. Arch Gen Psychiatry 1989;46:1006-1011.
- Cooper J. The Leyton Obsessional Inventory. Psychol Med 1970;1: 48-64.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 1994. 4th ed. Washington: American Psychiatric Association; 1994.
- Hwang JP, Tsai SJ, Yang CH, Liu KM, Lirngt JF. Hoarding behavior in dementia, a preliminary report. Am J Geriatr Psychiatry 1998;6: 285-289.
- Homma A, Ishii T, Niina R. Relationship of behavioral complications and severity of dementia in Japanese elderly persons. Alzheimer Dis Assoc Disord 1994;8:46-53.
- Greenberg D, Witztum E, Levy A. Hoarding as a psychiatric symptom. J Clin Psychiatry 1990;51:417-421.
- Luchins DJ, Goldman MB, Lieb M, Hanrahan P. Repetitive behaviors in chronically institutionalized schizophrenic patients. Schizophr Res 1992;8:119-123.
- Frankenburg F. Hoarding in anorexia nervosa. Br J Med Psychol 1984;57:57-60.
- 12. Hellings JA, Warnock JK. Self-injurious behavior and serotonin in Prader-Willi Syndrome. Psychopharma Bull 1994;30:245-250.
- Sebit MB, Acuda W, Chibanda D. A case of the frontal lobe syndrome following head injury in Harare, Zimbabwe. Central Africa J Med 1996;42:51-53.
- Luchins DJ. A possible role of hippocampal dysfunction in schizo- phrenic symptomatology. Biol Psychiatry 1990,28:87-91.
- Adams PL. Obsessive children. New York: Brunner/Mazel; 1973.
- Thomas ND. Hoarding: eccentricity or pathology: when to intervene? J Gerontol Social Work 1997;29:45-55.
- Hogstel MO. Understanding hoarding behavior in the elderly. Am J Nurs 1993;July:42-45.
- Furby L. Possessions: toward a theory of their meaning and function throughout the life cycle. In: Bates PB, editor. Life span development and behavior. Vol 1. New York: Academic Press; 1978.
- Fromm E. Man for himself: an inquiry into the psychology of ethics. New York: Rhinehart; 1947.
- Frost RO, Hartl TL, Christian R, Williams N. The value of possessions in compulsive hoarding: patterns of use and attachment. Behav Res Ther 1995;33:897-902.
- Melamed Y, Szor H, Barak Y, Elizur A. Hoarding — what does it mean? Compr Psychiatry 1998;39:400-402.
- Frost RO, Hartl TL. A cognitive-behavioral model of compulsive hoarding. Behav Res Ther 1996;34:341-350.
- Chong SA, Tan CH, Lee HS. Hoarding and clozapine-risperidone combination. Can J Psychiatry 1996;41:315-316.
- Salzman L. The obsessive personality: origins, dynamics and therapy. New York: Jason Aronson; 1973.
- Hartl TL, Frost RO. Cognitive-behavioral treatment of compulsive hoarding: a multiple baseline experimental case study. Behav Res Ther 1999;37:451-461.
- Vostanis P, Dean C. Self-neglect in adult life. Br J Psychiatry 1992; 161:265-267.
- Greenberg D. Compulsive hoarding. Am J Psychotherapy 1987;XLI: 409-416.
- World Health Organization. International Classification of Diseases. 10th ed. Geneva: World Health Organization; 1992.
- Folstein MF, Folstein SE, McHugh, PR. Mini-mental State. A practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res 1975;12:189-198.
- Chiu H, Lee HC, Chung WS, Kwong PK. Reliability and validity of the Cantonese version of Mini-Mental State Examination — a preliminary study. HK J Psychiatry 1994;4(2):25-28.
- Spitzer RL, Endicott J, Fleiss JL, Cohen J. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976;33:766-771.