East Asian Arch Psychiatry 2018;28:3-8
ORIGINAL ARTICLE

Dr Cyrus SH Ho, Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore.
Dr Yanxia Lu, Department of Clinical Psychology and Psychiatry / School of Public Health, Zhejiang University College of Medicine, Hangzhou, China.
Dr Nenna Ndukewe, Department of Psychology, James Cook University, Singapore.
Dr Matilda WP Chew, Department of Paediatrics, National University Hospital, Singapore.
Dr Asim Shabbir, Department of Surgery, Yong Loo Lin School of Medicine, National University of Singapore.
Dr Jimmy BY So, Department of Surgery, Yong Loo Lin School of Medicine, National University of Singapore.
Dr Roger CM Ho, Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore.
Address for correspondence: Dr Cyrus SH Ho, Department of Psychological Medicine, Level 9, NUHS Tower Block, 1E Kent Ridge Road, Singapore 119228. Email:su_hui_ho@nuhs.edu.sg
Submitted: 29 March 2017; Accepted: 7 November 2017
Abstract
Background: Obesity is a major component of metabolic syndrome and an independent risk factor for various chronic diseases. It is also closely associated with mental illness, and the interaction is complex and multifactorial. This study aimed to estimate the prevalence of anxiety and depressive symptoms among obese Singaporeans.
Methods: Cross-sectional data of 36 male and 47 female obese Singaporeans who had been referred to the weight management clinic of National University Hospital, Singapore, between January 2010 and November 2011 were collected. Obesity was classified according to criteria of the World Health Organization. The extents of anxiety and depressive symptoms were measured using the Hospital Anxiety and Depression Scale.
Results: In obese Singaporeans attending the weight management clinic, the prevalence of anxiety symptoms was higher than that of depressive symptoms (28% vs 11%). There was no major socioeconomic difference between obese patients with and without anxiety, or with and without depressive symptoms. Conclusion: In obese Singaporeans, anxiety symptoms may be more common than depressive symptoms. Weight management programmes should incorporate anxiety management as part of standard treatment. Early detection and pharmacological and psychological interventions should be implemented.
Key words: Anxiety; Depression; Obesity; Prevalence
Introduction
Obesity is a global public health problem whose prevalence has increased over the years, along with obesity-related major disabilities and premature deaths.1 In 2008, the World Health Organization (WHO) estimated that globally approximately 1.5 billion adults were overweight (body mass index [BMI], 25-30 kg/m2) and about 500 million people were obese (BMI >30 kg/m2).2 By 2015, the respective figures were estimated to be 2.3 billion and >700 million.2
According to the Singapore National Health Survey, the prevalence of obesity among adults aged 18 to 69 years increased to 10.8% in 2010,3 from 6.9% in 2004.4 Singapore has a population of about 5.1 million and comprises the following ethnic groups: Chinese (74.1%), Malay (13.4%), Indian (9.2%), and others (3.3%).3 There are significant ethnic differences in obesity, with the rate being highest in Malays (24.0%), followed by Indians (16.9%) and Chinese (7.9%).3
Obesity is a major component of metabolic syndrome; others include elevated blood pressure, hypertriglyceridaemia, low serum level of high-density lipoprotein cholesterol, and high fasting serum level of glucose. All are independent risk factors for diabetes, coronary heart disease, and cerebrovascular disease. Metabolic syndrome affects approximately 20% to 25% of the population worldwide and is associated with a two- fold increase in the risk of death and three-fold increase in the risk of heart attack or stroke, compared with healthy individuals.5 It inevitably results in a substantial health care burden.
Psychological factors may influence the development and treatment of obesity, although results have been conflicting, especially between western and Asian populations.6 In a study of 9125 representative samples in the United States, obesity was associated with a significant increase in lifetime diagnosis of major depression, bipolar disorder, panic disorder, and agoraphobia.7 Similarly, obesity was reported to be associated with a higher risk of mood and anxiety disorders, even after adjusting for age and sex.8 In a longitudinal study of adolescent females, obesity was a predictor of depression.9 Depression was
Various mechanisms have been postulated to explain the complex and multifactorial interaction between obesity and mental disorders. Patients with depression and anxiety are less likely to abide by dietary restrictions and more likely to be socially isolated and physically inactive. They tend to adopt unhealthy habits such as smoking and alcohol misuse. This behaviour contributes to obesity and subsequent insulin resistance.14 The lack of exercise may also decrease serotonin synthesis and worsen depression and anxiety. The psychological stress associated with stigmatisation and low self-esteem in obese persons may in turn worsen depressive and anxiety symptoms.
Furthermore, activation of the hypothalamic- pituitary-adrenal axis increases levels of cortisol.15 Chronic elevation of plasma cortisol levels can lead to pseudo- Cushing syndrome, which is characterised by increased visceral adiposity, hyperinsulinaemia, insulin resistance, hypertension, and dyslipidaemia; all are hallmarks of metabolic syndrome. The chronic increase in insulin and leptin may activate the sympathetic nervous system and elevate the circulating catecholamine level, leading to faulty glucose metabolism, abdominal fat accumulation, and poor blood pressure regulation.16,17 The increased levels of pro- inflammatory cytokines18 and leptin resistance19 in obese patients are also associated with depressive disorder.
The comorbidity of depression with a chronic disease incrementally worsens health outcomes, compared with depression alone or any chronic disease alone, or any combination of chronic diseases without depression.20 Most studies of obesity and psychiatric symptoms have been based on western societies.21-23 Studies in Asians are scarce. This study aimed to estimate the prevalence of anxiety and depressive symptoms among obese Singaporeans. We hypothesised that patients with higher levels of obesity would have a higher prevalence of depressive and anxiety symptoms.
Methods
This study was approved by the National University of Singapore Institutional Review Board. Between January 2010 and November 2011, all patients with obesity who had been referred by primary care physicians or other specialists for weight management at the National University Hospital, Singapore were recruited. Written informed consent was obtained from each patient who fulfilled the inclusion criteria and agreed to participate. The inclusion criteria were as follows: (1) Asian ethnicity (e.g. Chinese, Indian, or Malay), (2) a BMI of ≥30 kg/m2, and (3) no previous surgical treatment for obesity. The exclusion criteria were as follows: (1) age of <18 years or >65 years, (2) insufficient mental capacity to provide informed consent, (3) pregnancy, (4) current incarceration, and (5) presence of severe psychiatric disorders (eg, schizophrenia, bipolar disorder, substance abuse, or dementia). The sample size was not calculated before the study.
Data were collected by a trained research assistant. Sociodemographic information (age, sex, education, marital status, ethnicity, housing, employment status) and health behaviours (smoking, alcohol drinking, and physical activity level) were obtained using a self-report questionnaire. The BMI data were obtained from records collected at the first attendance to the weight management clinic. According to the WHO international classification of obesity, obesity was defined as BMI of ≥30 kg/m2 and categorised as class I (moderate, BMI of 30 to <35 kg/m2), class II (severe, BMI of 35 to <40 kg/m2), and class III (morbid, BMI of ≥40 kg/m2).24 The WHO classification system has been validated in the Chinese population.25
Levels of anxiety and depressive symptoms were measured using the self-administered Hospital Anxiety and Depression scale. A subscale score of ≤7 was classified as absence of anxiety or depression, 8-10 as borderline anxiety or depressive symptoms, and >10 as having anxiety or depressive symptoms. These cut-off points have a sensitivity and specificity of approximately 0.80 in the diagnosis of clinical anxiety or depression in a hospital setting.26 The Hospital Anxiety and Depression scale has been used to assess severity of anxiety or depressive symptoms in patients with diabetes27 and metabolic syndrome.28 It has been validated in medical out-patients in Singapore; the anxiety subscale was more reliable than the depression subscale (Cronbach’s alpha, 0.83 and 0.85 for the anxiety subscale in men and women, respectively, vs 0.62 and 0.77 for the depression subscale in men and women, respectively).29
Statistical analyses were performed using SPSS (Windows version 11.5; SPSS, Chicago [IL], US). Two- sided hypothesis testing with an alpha level of <0.05 was used. Analyses were performed separately for men and women to avoid effect modification by sex.30 Differences in demographic data were examined using the chi-square test for categorical variables. Analysis of variance was used to compare the anxiety and depression subscale scores across different demographic and socioeconomic subgroups.
Results
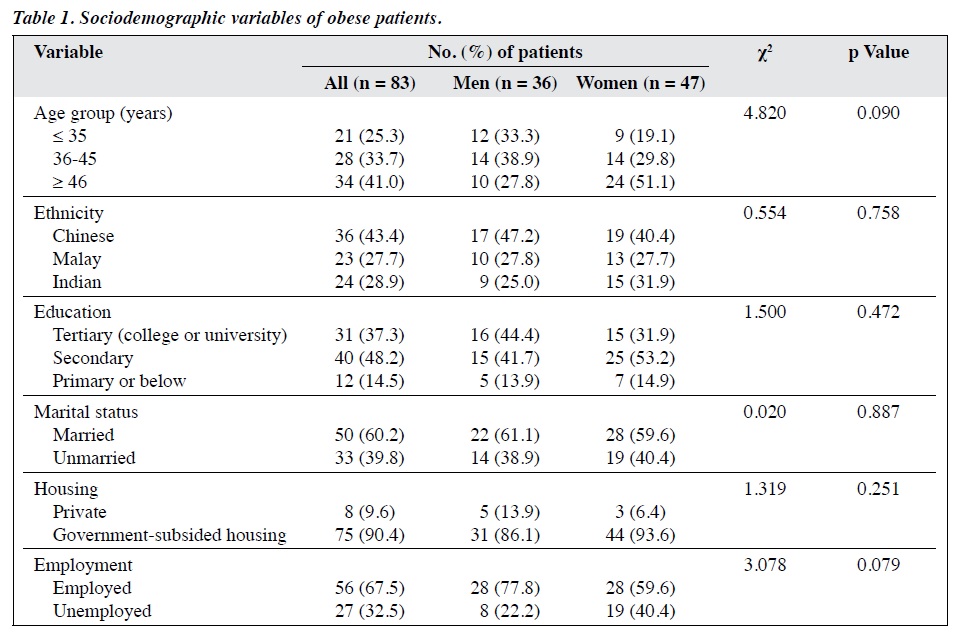
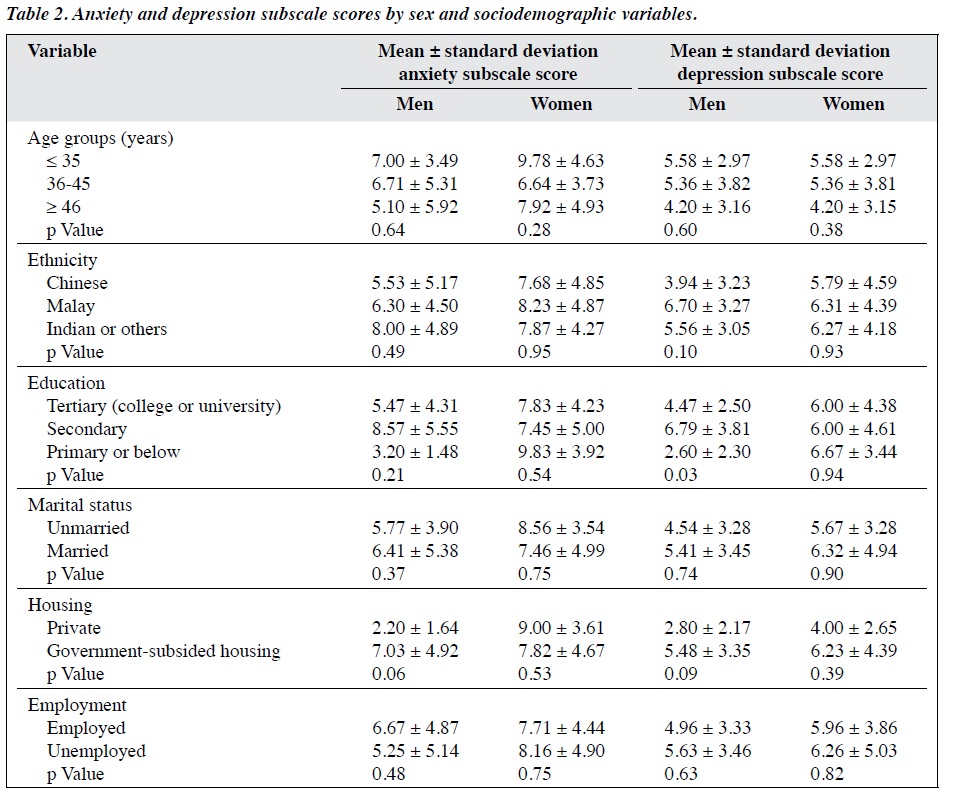
A total of 36 male and 47 female patients were included. Most were Chinese (43%), followed by Malay (28%) and Indian or other (29%). Over 85% had attained at least secondary education, and over 60% were married and employed (Table 1). Men with secondary education had a significantly higher mean depression subscale score than those with primary or tertiary education (p = 0.03, Table 2). No other sociodemographic factors were significantly associated with the mean anxiety and depression subscale
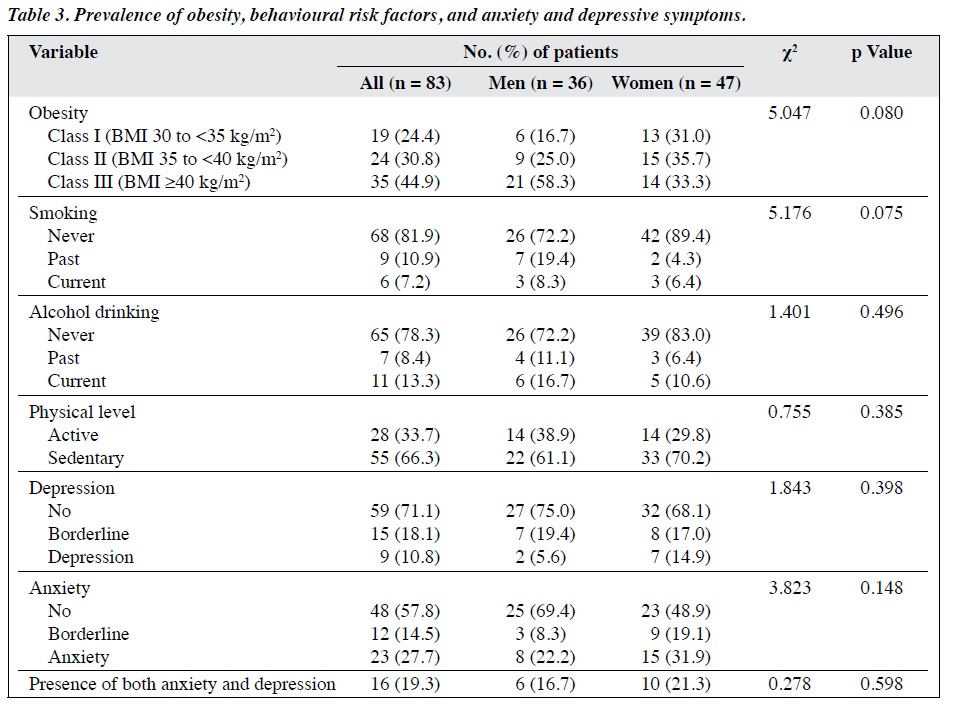
scores. The proportions of class I, class II, and class III obesity were 17%, 25%, and 58% in men and 31%, 36%, and 33% in women, respectively (Table 3).
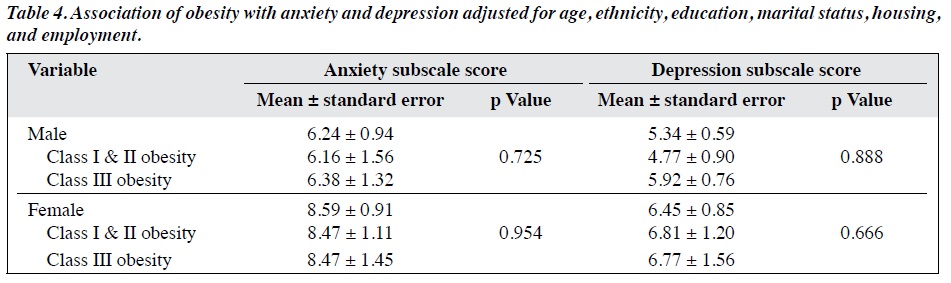
The prevalence of anxiety and borderline anxiety was 28% and 15%, respectively. The prevalence of depression and borderline depression was 11% and 18%, respectively. There was no significant difference by sex for prevalence of anxiety and depression. The mean anxiety and depression subscale scores did not differ significantly in different subgroups of age, ethnicity, education, marriage, housing, or employment (Table 4).
Discussion
To the best of our knowledge, this is the first study to determine the prevalence and severity of anxiety and depressive symptoms in obese Singaporeans. One study reported that being overweight increased the depression score among the more educated but not the less educated,31 although another study reported otherwise.32 In our study, men with secondary education had a significantly higher mean depression subscale score than those with primary or tertiary education. We hypothesise that men with secondary education are more health conscious and have a better understanding of health, but less economic and social resources for mental health is allocated to them than to those with tertiary education. Nonetheless, our sample was small and there were no specific questionnaires to assess patient health consciousness.
In this sample of obese Singaporeans, the prevalence of anxiety symptoms was higher than that of depressive symptoms (28% vs 11%). This finding is consistent with those of studies that report obese patients as having increased anxiety symptoms besides depressive symptoms,33,34 although depressive symptoms are usually more prominent.35 The higher prevalence of anxiety than depressive symptoms in our patients could be due to several reasons. First, anxiety may not affect a person the way depression does, and more people may have had untreated anxiety than depression in our sample. Second, obesity may increase body dissatisfaction and decrease self-esteem and cause anticipatory and social anxiety. Detrimental effects of obesity on self-esteem and social anxiety have been illustrated in an adolescent sample from China.36 In a Singaporean study of chronic inflammatory rheumatological diseases, those with physically stigmatising disorders such as systemic lupus erythematous had a higher anxiety score but not depression score after controlling for potential confounders, compared with disorders such as gout and rheumatoid arthritis.37 Similarly, obesity can lead to acute stress, social impairment, and low satisfaction with life, and thus increase the level of anxiety. In addition, underlying depression could drive this association, as depression and anxiety are highly comorbid. Asians may be more comfortable reporting anxiety than depressive symptoms. Association studies of obesity and anxiety are limited,
compared with those of obesity and depression.38,39 Thus, recognising the effects of anxiety on obesity is necessary.
In our study, we observed no major socioeconomic differences between obese patients with and without anxiety, or with and without depressive symptoms, probably due to the limited sample size. High levels of anxiety symptoms have been found to be associated with elevated risks for coronary heart disease and sudden cardiac death in both men and women.28,40,41 Thus, the cardiovascular status of obese patients should be monitored, especially those with anxiety symptoms. Because anxiety may be more commonly encountered (than depression) by obese Singaporeans, weight management programmes should incorporate comprehensive anxiety management, including psychoeducation, adjustment of self-perception, teaching of relaxation techniques, and cognitive behaviour therapy.
Our study had several limitations. The sample was small and thus findings were preliminary. The prevalence of anxiety and depressive symptoms may have been high because patients were recruited from a secondary-care centre and may have a more complicated course than those in the community. Populations of most East Asian countries are rather homogeneous; hence, multicentre studies are required to study ethnic differences. Anxiety and depressive symptoms were assessed by a self-administered questionnaire rather than a diagnostic interview. Thus, no clinical diagnosis of anxiety disorder or depressive disorder was made. Anxiety and depressive symptoms measured by self-administered questionnaires are more prone to convergence, compared with a diagnosis made by a diagnostic interview.42 Nevertheless, the use of a self-administered questionnaire to study the relationship between depression and diabetes has been reported to be acceptable if the questionnaire is well validated, particularly for medical or surgical patients.30 As the Hospital Anxiety and Depression scale reflects anxiety and depressive symptoms during the previous week,28 the prevalence of lifetime anxiety or depression may have been underestimated. Finally, because measurement was performed at a single timepoint, our findings did not allow us to draw conclusions on causality. A prospective study is required to evaluate the effect of intervention on psychiatric symptoms in obese patients.
Conclusion
In obese Singaporeans, the prevalence of anxiety symptoms may be higher than that of depressive symptoms. Weight management programmes should therefore incorporate anxiety management as part of standard treatment.
Acknowledgements
We thank the Department of Psychological Medicine, National University of Singapore and the Weight Management Clinic of the National University Hospital for their support.
Declaration
The authors have no conflicts of interest to disclose.
References
- Teo EY, Lew PS, Foo CS. Public perceptions of obesity and bariatric surgery in Singapore: a pilot study. Singapore Med J 2012;53:104-8.
- World Health Organization. Obesity and Overweight Fact Sheet. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed 22 Jan 2017.
- Singapore, Ministry of Health, Epidemiology & Disease Control Division. National Health Survey. 2010. Available from https://www.moh.gov.sg/content/dam/moh_web/Publications/Reports/2011/NHS2010%20-%20low%20res.pdf. Accessed 23 Jan 2017.
- Singapore, Ministry of Health, Epidemiology & Disease Control Division. National Health Survey. 2004. p. 26. Available from http://www.moh.gov.sg/content/dam/moh_web/Publications/ Reports/2005/1/NHS_2004%28Part4%29.pdf. Accessed 22 Jan 2017.
- International Diabetes Federation (2006) International Diabetes Federation Consensus Worldwide Definition of the Metabolic Syndrome. Available from: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome. Accessed 22 Feb 2017.
- Subramaniam M, Picco L, He V, Vaingankar JA, Abdin E, Verma S, et al. Body mass index and risk of mental disorders in the general population: results from the Singapore Mental Health Study. J Psychosom Res 2013;74:135-41. cross ref
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry 2006;63:824-30. cross ref
- Scott KM, McGee MA, Wells JE, Oakley Browne MA. Obesity and mental disorders in the adult general population. J Psychosom Res 2008;64:97-105. cross ref
- Boutelle KN, Hannan P, Fulkerson JA, Crow SJ, Stice E. Obesity as a prospective predictor of depression in adolescent females. Health Psychol 2010;29:293-8. cross ref
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 1997;349:1498-504. cross ref
- 1 Atlantis E, Baker M. Obesity effects on depression: systematic review of epidemiological studies. Int J Obes (Lond) 2008;32:881-91. cross ref
- Hu HY, Wu CY, Chou YJ, Huang N. Body mass index and mental health problems in general adults: disparity in gender and socioeconomic status. J Psychosom Res 2012;72:393-8. cross ref
- Kim E, Song JH, Hwang JY, Ahn K, Kim J, Koh YH, et al. Obesity and depressive symptoms in elderly Koreans: evidence for the “Jolly Fat” hypothesis from the Ansan Geriatric (AGE) Study. Arch Gerontol Geriatr 2010;51:231-4. cross ref
- Attvall S, Fowelin J, Lager I, Von Schenck H, Smith U. Smoking induces insulin resistance--a potential link with the insulin resistance syndrome. J Intern Med 1993;233:327-32. cross ref
- Bjömtorp P, Rosmond R. The metabolic syndrome – a neuroendocrine disorder? Br J Nutr 2000;83(Suppl 1):S49-57.
- Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998;55:580-92. cross ref
- Anagnostis P, Athyros VG, Tziomalos K, Karagiannis A, Mikhailidis DP. Clinical review: the pathogenetic role of cortisol in the metabolic syndrome: a hypothesis. J Clin Endocrinol Metab 2009;94:2692-701. cross ref
- Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1 and IL-6: a meta-analysis. Psychosom Med. 2009;71:171-86. cross ref
- Patel SB, Reams GP, Spear RM, Freeman RH, Villarreal D. Leptin: linking obesity, the metabolic syndrome, and cardiovascular disease. Curr Hypertens Rep 2008;10:131-7. cross ref
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007;370:851-8. cross ref
- Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J Psychosom Res 2002;53:891-5. cross ref
- Green AJ, Bazata DD, Fox KM, Grandy S. Quality of life, depression, and healthcare resource utilization among adults with type 2 diabetes mellitus and concomitant hypertension and obesity: a prospective survey. Cardiol Res Pract 2012;2012:404107. cross ref
- Labad J, Price JF, Strachan MW, Fowkes FG, Ding J, Deary IJ, et al. Symptoms of depression but not anxiety are associated with central obesity and cardiovascular disease in people with type 2 diabetes: the edinburgh type 2 diabetes study. Diabetologia 2010;53:467-71. cross ref
- Ravussin E, Swinburn BA. Pathophysiology of obesity. Lancet 1992;340:404-8. cross ref
- Reynolds K, Gu D, Whelton PK, Wu X, Duan X, Mo J, et al. Prevalence and risk factors of overweight and obesity in China. Obesity (Silver Spring) 2007;15:10-8. cross ref
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69-77. cross ref
- Gois C, Dias VV, Raposo JF, do Carmo I, Barbosa A. Vulnerability to stress, anxiety and depressive symptoms and metabolic control in type 2 diabetes. BMC Res Notes 2012;5:271. cross ref
- Skilton MR, Moulin P, Terra JL, Bonnet F. Associations between anxiety, depression, and the metabolic syndrome. Biol Psychiatry 2007;62:1251-7. cross ref
- Ho RC, Fu EH, Chua AN, Cheak AA, Mak A. Clinical and psychosocial factors associated with depression and anxiety in Singaporean patients with rheumatoid arthritis. Int J Rheum Dis 2011;14:37-47. cross ref
- Adriaanse MC, Dekker JM, Heine RJ, Snoek FJ, Beekman AJ, Stehouwer CD, et al. Symptoms of depression in people with impaired glucose metabolism or type 2 diabetes mellitus: The Hoorn Study. Diabet Med 2008;25:843-9. cross ref
- Ross CE. Overweight and depression. J Health Soc Behav 1994;35:63-79. cross ref
- Kranjac AW, Nie J, Trevisan M, Freudenheim JL. Depression and body mass index, differences by eductaion: evidence from a population- based study of adult women in the U.S. Buffalo-Niagara region. Obes Res Clin Pract 2017;11:63-71. cross ref
- Lin HY, Huang CK, Tai CM, Lin HY, Kao YH, Tsai CC, et al. Psychiatric disorders of patients seeking obesity treatment. BMC Psychiatry 2013;13:1. cross ref
- de Wit LM, Fokkema M, van Straten A, Lamers F, Cuijpers P, Penninx BW. Depressive and anxiety disorders and the association with obesity, physical, and social activities. Depress Anxiety 2010;27:1057-65. cross ref
- Lykouras L. Psychological profile of obese patients. Dig Dis 2008;26:36-9. cross ref
- C Jiao, D Yan, T Wang. Weight perception, body size, self-esteem and social anxiety in obese adolescents: a Multiple Indicators Multiple Causes (MIMIC) model. Int J Psychol Behav Sci 2016;6:1-6.
- Mak A, Tang CS, Chan MF, Cheak AA, Ho RC. Damage accrual, cumulative glucocorticoid dose and depression predict anxiety in patients with systemic lupus erythematosus. Clin Rheumatol 2011;30:795-803. cross ref
- Becker ES, Margraf J, Türke V, Soeder U, Neumer S. Obesity and mental illness in a representative sample of young women. Int J Obes Relat Metab Disord 2001;25(Suppl 1):S5-9. cross ref
- Goldstein LT, Goldsmith SJ, Anger K, Leon AC. Psychiatric symptoms in clients presenting for commercial weight reduction treatment. Int J Eat Disord 1996;20:191-7. cross ref
- Albert CM, Chae CU, Rexrode KM, Manson JE, Kawachi I. Phobic anxiety and risk of coronary heart disease and sudden cardiac death among women. Circulation 2005;111:480-7. cross ref
- Kawachi I, Sparrow D, Vokonas PS, Weiss ST. Symptoms of anxiety and risk of coronary heart disease. The Normative Aging Study. Circulation 1994;90:2225-9. cross ref
- Hermanns N, Kulzer B, Krichbaum M, Kubiak T, Haak T. How to screen for depression and emotional problems in patients with diabetes: comparison of screening characteristics of depression questionnaires, measurement of diabetes-specific emotional problems and standard clinical assessment. Diabetologia 2006;49:469-77. cross ref


