East Asian Arch Psychiatry 2022;32:39-42 | https://doi.org/10.12809/eaap20104
ORIGINAL ARTICLE
WM Metekiya, Department of Psychiatry, College of Health Sciences, Mekelle University, Mekelle, Ethiopia
AT Gebreselassie, Department of Psychiatry, College of Health Sciences, Mekelle University, Mekelle, Ethiopia
TA Amare, Department of Psychiatry, College of Health Sciences, Mekelle University, Mekelle, Ethiopia
DZ Wondafrash, Department of Pharmacology, Saint Pauls Hospital Millennium Medical College, Addis Ababa, Ethiopia
Address for correspondence: WM Metekiya, Department of Psychiatry, College of Health Sciences, Mekelle University, Mekelle, Ethiopia. Email: workua.mekonen@mu.edu.et
Submitted: 31 October 2020; Accepted: 27 May 2022
Abstract
Background: People with human immunodeficiency virus (HIV) are at higher risk of suicidal ideation and suicide attempts. We reviewed the literature for the prevalence and determinants of suicidal ideation and suicide attempt in people with HIV in Africa.
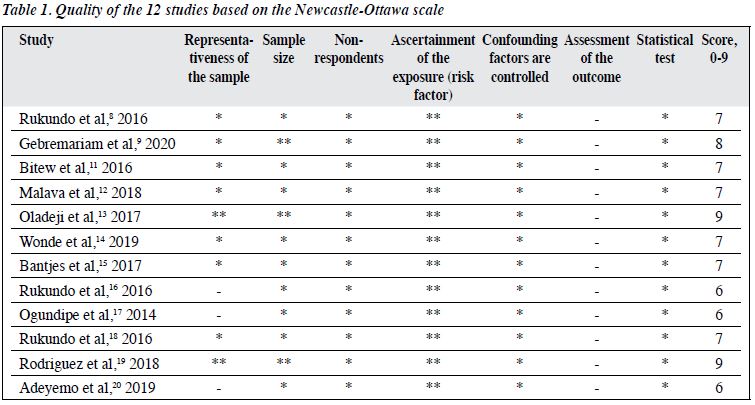
Methods: The PubMed, Scopus, and Google scholar were searched for original studies published in peer- reviewed journals in English language between January 2015 to July 2020, using the key words: ‘suicidal behavior’, ‘suicidal attempt’, ‘suicidal ideation’, ‘HIV/AIDS’, and/or ‘Africa’. The quality of included studies was assessed using the Newcastle-Ottawa scale.
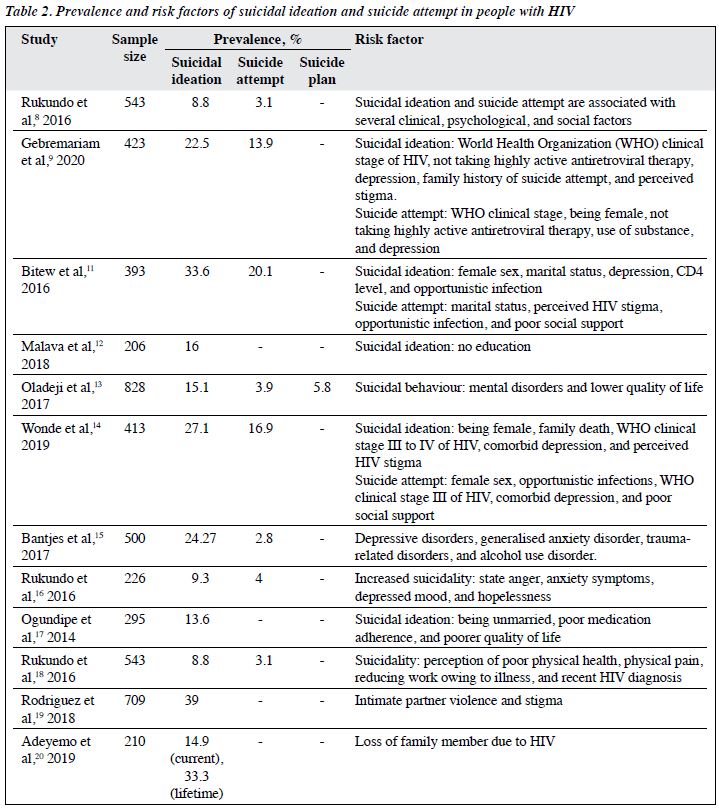
Results: 12 cross-sectional studies published in the past 5 years in African countries were included. The quality of studies was high, with score ranging from 6 to 9. The prevalence of suicidal ideation ranged from 8.8% to 39%. The prevalence of suicide attempt ranged from 2.8% to 20.1%. The most common risk factors for suicidal behaviour were mental health-related problems. Other factors included high clinical stage of HIV, being unmarried, poor medication adherence, poorer quality of life, not taking highly active antiretroviral therapy, female sex, no education, substance use, low CD4 level, and opportunistic infection.
Conclusion: Patients with HIV/AIDS have an increased risk of suicidal ideation and suicide attempts. Early screening, treatment, and referral of suicidal patients are necessary for HIV clinics.
Key words: Acquired Immunodeficiency Syndrome; Africa; HIV; Suicidal ideation; Suicide; Suicide, attempted
Introduction
Suicidal behaviour and human immunodeficiency virus (HIV) / acquired immune deficiency syndrome (AIDS) are major public health issues, particularly in low- and middle-income countries.1 Patients with HIV/AIDS are at higher risk for suicidal behaviour.2,3 Such patients have 6.55 times higher risk of suicidal ideation, compared with the general population, and have higher risks of suicide and accidental or violent death.4 In Brazil, the suicide risk was 56% among patients with a chronic illness and was 5.24 times higher in patients with HIV than in those without a medical condition.5
People with chronic illnesses, particularly HIV/AIDS are at increased risk of suicide.6 In South Africa, 83.1% of patients with HIV/AIDS had a significantly elevated risk of suicidal ideation, and most of them were young men aged <30 years.7 Two time points are peak for suicide incidence: 72 hours and 6 weeks after the diagnosis of HIV/AIDS, in addition to immediately after the diagnosis.7 In Uganda, the rate of suicidal ideation was 8.8% and the rate of suicide attempt was 3.1% in patients with HIV/AIDS, and thus assessment and management of suicide risk is an integral part of HIV care.8 In people with HIV, the prevalence of suicidal ideation has been reported to vary from 13.6% to 31.0%, and the prevalence of attempted suicides has been reported to vary from 3.9% to 32.7%.9 In Ethiopia, the respective prevalence was 22.5% and 13.9%; people with HIV/AIDS face various day-to-day and long-term personal, interpersonal, social, physical, and psychological challenges in addition to health conditions.9 We aimed to review the literature for the prevalence and determinants of suicidal ideation and suicide attempt in people with HIV in Africa.
Methods
The databases of PubMed, Scopus, and Google scholar were searched for original studies published in peer-reviewed journals in English language between January 2015 to July 2020, using the key words: ‘suicidal behavior’, ‘suicidal attempt’, ‘suicidal ideation’, ‘HIV/AIDS’, and/or ‘Africa’. Studies on non-suicidal deliberate self-harm were excluded, as were studies with only the abstract available. The title and abstract of each study were screened by two authors independently for eligibility. Disagreements between the two authors were resolved by consensus of the remaining authors. Full text of eligible studies was then screened, and studies that did not fulfil the inclusion criteria were excluded.
Variables of included studies were extracted: citation of the study, country where the study was performed, year of data collection, study design, study population, age of participants, selection criteria of participants, prevalence of suicidal ideation, prevalence of attempted suicide, prevalence of completed suicide, method of data analysis, and sampling criteria for participants.
The quality of included studies was assessed by two authors independently using the Newcastle-Ottawa scale.10
The scale takes into account the representativeness of the sample, sample size, non-respondents, ascertainment of the exposure, and assessment of outcome.
Results
Of 868 studies identified, 13 were duplicates. Of 855 studies screened, 830 were excluded because of irrelevancy to the topic. Full text of 25 studies was screened for eligibility; 13 did not fulfil the inclusion criteria and were excluded. The remaining 12 were included in analysis.8,9,11-20 All 12 studies were cross-sectional studies published in the past 5 years in African countries. The quality of studies was high, with score ranging from 6 to 9 (Table 1). The prevalence of suicidal ideation ranged from 8.8% to 39%, whereas the prevalence of suicide attempt ranged from 2.8% to 20.1% (Table 2). The most common risk factors for suicidal behaviour were mental health-related problems. Other risk factors included high clinical stage of HIV, being unmarried, poor medication adherence, poorer quality of life, not taking highly active antiretroviral therapy, female sex, no education, substance use, low CD4 level, and opportunistic infection.
Discussion
People with HIV/AIDS have higher prevalence of suicidal behaviour (suicidal ideation and suicide attempt), compared with those HIV-negative. Suicidal ideation is a predictor for attempted and completed suicide in adolescents with HIV.8 Suicidal behaviour occurs in all stages of HIV infection. In the present review, the prevalence of suicidal ideation was 8.8% to 39%, whereas the prevalence of suicide attempt was 2.8% to 20.1.8,9,11-20 In a review in the United Kingdom, the prevalence was 26.9% for suicidal ideation, 30.2% for suicidal thoughts, and 22.2% for a suicide plan.21 In Italy, the prevalence of suicidal ideation was 13.6% to 31.0%, whereas the prevalence of attempted suicide was 3.9% to 32.7%.22 In women with HIV during pregnancy and postpartum, the prevalence of suicidal ideation was 39% prenatally and 7% at 12 months postpartum; 13% experienced incident suicidal ideation.23
One risk factor for suicidal behaviour is being women. Women tend to internalise stressful events, whereas men tend to act them out.7 In addition, the high World Health Organization clinical stage of AIDS is a risk factor for suicide attempts. This may be because patients with advanced immunosuppression may have opportunistic infections that may lead to suicide attempts.9 In addition, patients who do not take highly active antiretroviral therapy may have concerns on lifelong drug adverse effects and the burden of lifelong treatment.9 Substance use may disturb the normal function of the brain and result in attempted suicide, particularly when patients are unable to buy the substance.18 Social stigmatisation regards HIV/AIDS as a terminal illness, which imposes an enormous emotional and psychological burden on the patient and family.17 Intimate partner violence and depression are predictors for sustained suicidal ideation, whereas increased income, younger age, disclosure of HIV status to partner, and greater stigma are predictors for incident suicidal ideation.21
Healthcare providers should be aware of suicidal behaviour in patients with HIV. They should routinely assess the patients’ suicidal behaviour, depressive symptoms, and common mental illness, and refer to mental health services if needed. Treating depression can improve the suicidality and the CD4 count. Further studies are warranted to determine the cause-effect relationships between suicidal behaviour and HIV viral load, CD4 count, treatment outcome, and quality of life among people with HIV.
Conclusion
Patients with HIV/AIDS have an increased risk of suicidal ideation and suicide attempts. Early screening, treatment, and referral of suicidal patients are necessary for HIV clinics.
Contributors
All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability
All data generated or analysed during the present study are available from the corresponding author on reasonable request.
References
- Liu Y, Niu L, Wang M, Chen X, Xiao S, Luo D. Suicidal behaviors among newly diagnosed people living with HIV in Changsha, China. AIDS Care 2017;29:1359-63. Crossref
- Govender RD, Schlebusch L. Suicidal ideation in seropositive patients seen at a South African HIV voluntary counselling and testing clinic. Afr J Psychiatry (Johannesbg) 2012;15:94-98. Crossref
- Ahmedani BK, Peterson EL, Hu Y, et al. Major physical health conditions and risk of suicide. Am J Prev Med 2017;53:308-15. Crossref
- McManus H, Petoumenos K, Franic T, et al. Determinants of suicide and accidental or violent death in the Australian HIV Observational Database. PLoS One 2014;9:e89089. Crossref
- Guimarães PM, Passos SR, Calvet GA, Hökerberg YH, Lessa JL, Andrade CA. Suicide risk and alcohol and drug abuse in outpatients with HIV infection and Chagas disease. Bras J Psychiatry 2014;36:131-7. Crossref
- Kelbert EF, Pinheiro LM, Souza LDM, et al. Suicide risk in people living with AIDS/HIV: the effect of childhood trauma is mediated by mental disorders and social vulnerability. AIDS Care 2020;32:512-7. Crossref
- Schlebusch L, Govender RD. Elevated risk of suicidal ideation in HIV- positive persons. Depress Res Treat 2015;2015:609172. Crossref
- Rukundo GZ, Mishara BL, Kinyanda E. Burden of suicidal ideation and attempt among persons living with HIV and AIDS in semiurban Uganda. AIDS Res Treat 2016;2016:3015468. Crossref
- Gebremariam EH, Reta MM, Nasir Z, Amdie FZ. Prevalence and associated factors of suicidal ideation and attempt among people living with HIV/AIDS at Zewditu Memorial Hospital, Addis Ababa, Ethiopia: a cross-sectional study. Psychiatry J 2017;2017:2301524. Crossref
- Modesti PA. Cross sectional study Newcastle - Ottawa quality assessment scale. PLoS One 2016;11:1-2.
- Bitew H, Andargie G, Tadesse A, Belete A, Fekadu W, Mekonen T. Suicidal ideation, attempt, and determining factors among HIV/AIDS patients, Ethiopia. Depress Rese Treat 2016;2016:8913160. Crossref
- Malava JK, Lancaster KE, Hosseinipour MC, et al. Prevalence and correlates of probable depression diagnosis and suicidal ideation among patients receiving HIV care in Lilongwe, Malawi. Malawi Med J 2018;30:236-42. Crossref
- Oladeji BD, Taiwo B, Mosuro O, et al. Suicidal behavior and associations with quality of life among HIV-infected patients in Ibadan, Nigeria. J Int Assoc Provid AIDS Care 2017;16:376-82. Crossref
- Wonde M, Mulat H, Birhanu A, Biru A, Kassew T, Shumet S. The magnitude of suicidal ideation, attempts and associated factors of HIV positive youth attending ART follow ups at St. Paul’s Hospital Millennium Medical College and St. Peter’s specialized hospital, Addis Ababa, Ethiopia, 2018. PLoS One 2019;14: e0224371. Crossref
- Bantjes J, Kagee A, Saal W. Suicidal ideation and behaviour among persons seeking HIV testing in peri-urban areas of Cape Town, South Africa: a lost opportunity for suicide prevention. AIDS Care 2017;29:919-27. Crossref
- Rukundo GZ, Mishara B, Kinyanda E. Psychological correlates of suicidality in HIV/AIDS in semi-urban south-western Uganda. Trop Doct 2016;46:211-5. Crossref
- Ogundipe OA, Olagunju AT, Adeyemi JD. Suicidal ideation among attendees of a West African HIV clinic. Arch Suicide Res 2015;19:103-16. Crossref
- Rukundo GZ, Kinyanda E, Mishara B. Clinical correlates of suicidality among individuals with HIV infection and AIDS disease in Mbarara, Uganda. Afr J AIDS Res 2016;15:227-32. Crossref
- Rodriguez VJ, Cook RR, Peltzer K, Jones DL. Prevalence and psychosocial correlates of suicidal ideation among pregnant women living with HIV in Mpumalanga Province, South Africa. AIDS Care 2017;29:593-7. Crossref
- Adeyemo S, Olorunkoya OG, Chinelo OL, Abiri GB, Abojei CO. Prevalence and psychosocial correlates of suicidal ideation among adolescents living with HIV in Southwestern Nigeria, West Africa. HIV AIDS Rev 2019;18:273-8. Crossref
- Catalan J, Harding R, Sibley E, Clucas C, Croome N, Sherr L. HIV infection and mental health: suicidal behaviour--systematic review. Psychol Health Med 2011;16:588-611. Crossref
- Serafini G, Montebovi F, Lamis DA, et al. Associations among depression, suicidal behavior, and quality of life in patients with human immunodeficiency virus. World J Virol 2015;4:303-12. Crossref
- Rodriguez VJ, Mandell LN, Babayigit S, Manohar RR, Weiss SM, Jones DL. Correlates of suicidal ideation during pregnancy and postpartum among women living with HIV in rural South Africa. AIDS Behav 2018;22:3188-97. Crossref


