East Asian Arch Psychiatry 2022;32:47-50 | https://doi.org/10.12809/eaap2214
ORIGINAL ARTICLE
Karniza Khalid, Clinical Research Centre, Hospital Tuanku Fauziah, Perlis, Ministry of Health Malaysia
Yit Tyse Ooi, Department of Psychiatry and Mental Health, Hospital Tuanku Fauziah, Perlis, Ministry of Health Malaysia
Qutbuddin Abdul Rashid, Department of Psychiatry and Mental Health, Hospital Tuanku Fauziah, Perlis, Ministry of Health Malaysia
Muhammad Zul Azri Mohammad Yusoff, Department of Psychiatry and Mental Health, Hospital Tuanku Fauziah, Perlis, Ministry of Health Malaysia
Ruzita Jamaluddin, Clinical Research Centre & Department of Psychiatry and Mental Health, Hospital Tuanku Fauziah, Perlis, Ministry of Health Malaysia
Address for correspondence: Karniza Khalid, Clinical Research Centre, Hospital Tuanku Fauziah, Jalan Tun Abdul Razak, 01000 Kangar, Perlis, Malaysia. Email: karniza.khalid@moh.gov.my
Submitted: 28 February 2022; Accepted: 29 August 2022
Abstract
Objectives: To determine the prevalence of continued illicit drug use among people enrolled in methadone maintenance treatment (MMT), the association between hepatitis C status and methadone dosage, and the predictors for illicit drug abstinence during MMT.
Methods: Clinical records of active opioid dependents who underwent MMT between 1 January 2007 and 31 March 2021 in Hospital Tuanku Fauziah, Perlis, Malaysia were retrospectively reviewed. Data collected included baseline demographics, history of illicit drug use, temporal trend in methadone dosage modulation, and co-use of illicit drugs during the MMT.
Results: A total of 87 patients (mean age, 43.9 ± 8.33 years) were included. Their mean duration of involvement in MMT was 7.8 ± 3.69 years. The most commonly used drug was heroin (88.5%), followed by kratom (51.7%). Between 2019 and 2021, 61 (70.1%) patients had ceased abusing opioid, but 51 (58.6%) patients continued using any of the illicit drugs. Methamphetamine and amphetamine co-use was most common (n = 12, 37.5%). Hepatitis C status was not associated with the current methadone dose (U = 539.5, p = 0.186) or the highest dose required (t = -0.291, df = 74, p = 0.772). No predictor for illicit drug abstinence during MMT was identified. Methadone dose positively correlated with frequency of defaulting treatments (r = 0.22, p = 0.042).
Conclusion: Among our patients, MMT for opioid dependents cannot sufficiently curb illicit drug use, and there is a shift toward stimulants abuse.
Key words: Harm reduction; Illicit drugs; Methadone; Program evaluation; Retrospective studies
Introduction
According to the World Health Organization, illegal drug use is prevalent in 136 countries, of which 93 reported a high rate of HIV infection among intravenous drug users.1
Illegal drug use has claimed at least 11.8 million lives annually worldwide.2 The number of fatalities from drug abuse greatly outnumbers that from malignancy. Drug abuse can cause a lot of harm to the body physically and psychologically.3,4 Drug use may influence the person to act, feel, and think differently, especially in addiction. Methadone maintenance treatment (MMT) is indicated for people who are dependent on opioids or have a history of opioid dependence.5 However, in many countries, MMT is unavailable or illegal. For example, maintenance treatment by methadone and buprenorphine is forbidden in the Russian Federation although it has one of the highest rates of opioid users in the world; all treatment for drug abuse is abstinence oriented.5
Methadone is an opioid agonist; MMT aims to improve the health and social performance of opioid dependents, as people with addiction problems typically have a higher self- stigma level and poorer social functioning.6,7 In a systematic review of 38 articles, people on MMT engage in much less crime and have better employment rates and social functioning by being able to resume their roles in the family and society.8 Methadone has addictive potential, but being on methadone is not the same as being dependent on opioids such as heroin. It is safer for people to take methadone orally under medical supervision than to take heroin (often by injection) of unknown purity and risk HIV transmission if needles and syringes are shared.9 Methadone use in opioid addiction is considered an evidence-based treatment approach and is included in the World Health Organization List of Essential Medicines.10 This study aims to determine the prevalence of continued illicit drug use among people enrolled in MMT, the association between hepatitis C status and methadone dosage, and the predictors for illicit drug abstinence during MMT.
Materials and methods
This retrospective cohort study was approved by the Medical Research and Ethical Committee of the Ministry of Health Malaysia (reference: NMRR-21-206-58561). Clinical records of active opioid dependents who underwent MMT between 1 January 2007 and 31 March 2021 in Hospital Tuanku Fauziah, Perlis, Malaysia were retrospectively reviewed. Data collected included baseline demographics, history of illicit drug use, temporal trend in methadone dosage modulation, and co-use of illicit drugs during the MMT.
The sample size was calculated using the population proportion formulae.11 In a previous study, the prevalence of responders among opioid-dependent people undergoing MMT was 0.715.12 In our state-wide population of 90 heroin users on MMT, with both the preset type I error probability 10% for missing records or unavailable data, the minimum sample size required was 79. In another study, the proportion of opioid use was 0.69 among low-duration class and 0.30 among high-duration class.13 Thus, a minimum sample size of 25 per group was needed to reject the null hypothesis with 80% power. The type I error probability associated with this null hypothesis was 0.05. Chi-square test for independence was used to evaluate this null hypothesis. With an additional 20% accounting for missing data, a minimum sample size of 32 samples per group was required.
Statistical analysis was performed using SPSS (Windows version 26; IBM Corp, Armonk [NY], US). Normally distributed data were presented as mean and standard deviation, whereas skewed data were presented as median and interquartile range. Associations of hepatitis C status with the current methadone dose and the highest dose required were assessed using the Mann-Whitney U test and independent t-test, respectively. Correlation between methadone dose and frequency of defaulting treatment was assessed using Pearson correlation analysis. Multivariate analysis with logistic regression was used to identify predictors for drug abstinence during MMT.
Results
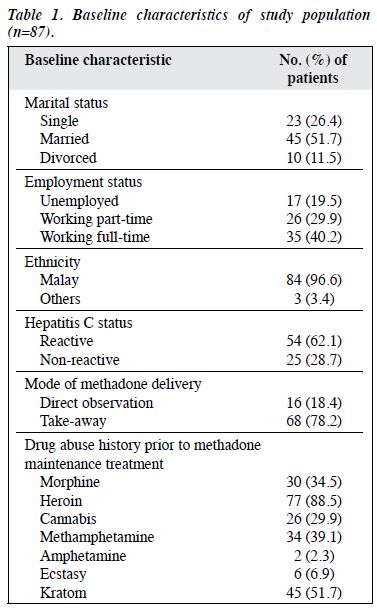
A total of 87 patients (mean age, 43.9 ± 8.33 years) were included (Table 1). Their mean duration of involvement in MMT was 7.8 ± 3.69 years. The mean methadone dosage was 22.4 ± 13.02 mg at the start and 42.2 ± 22.31 mg at present. 78% of patients were on take-away regimen.
The most commonly used drug was heroin (88.5%) with a mean duration of use of 12.5 ± 7.05 years before enrolment, followed by kratom (51.7%) with a mean duration of use of 8.3 ± 6.83 years before enrolment.
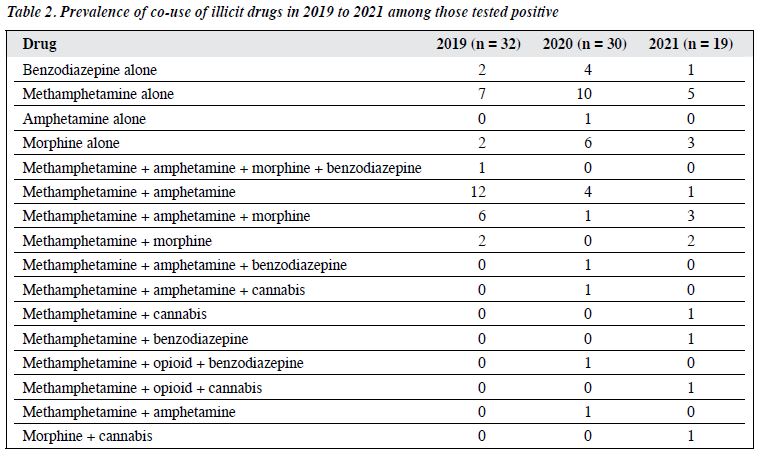
Between 2019 and 2021, 61 (70.1%) patients had ceased abusing opioid, but 51 (58.6%) patients continued using any of the illicit drugs; urine spot tests yielded the highest recorded positive cases in 2019 (n = 32, 36.8%), with methamphetamine and amphetamine co-use being most common (n = 12, 37.5%) [Table 2].
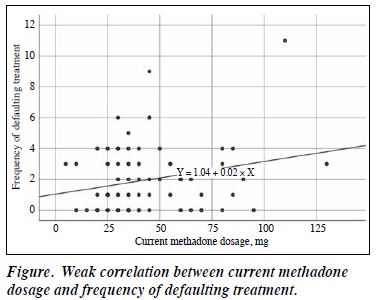
Among 54 (62.1%) patients with hepatitis C, the mean age at diagnosis was 36.7 ± 8.26 years, and most were diagnosed during routine medical work-up prior to enrolment into MMT. Hepatitis C status was not associated with the current methadone dose (U = 539.5, p = 0.186) or the highest dose required (t = -0.291, df = 74, p = 0.772). No predictor for illicit drug abstinence during MMT was identified. Methadone dose positively correlated with frequency of defaulting treatments (r = 0.22, p = 0.042, figure).
Discussion
In Malaysia, MMT was introduced in 2005 to reduce needle- borne HIV transmission among opioid abusers (so as to reduce the economic burden on HIV/AIDS treatment) and to curb the social ills associated with opioid dependence.5
However, 58.6% of our patients continued to use any of the illicit drugs during MMT, and there was a shift towards stimulants abuse.
Most patients were already diagnosed with hepatitis C prior to MMT, which suggests a long history of needle- sharing. Hepatitis C virus is associated with an increased risk of hepatocellular carcinoma.14 Most hepatitis C cases in Malaysia are caused by injection drug use, tattooing, body piercing, and vertical transmission.15 Treatment of hepatitis C infection involves immunomodulatory treatment with direct-acting antivirals, which are costly and limited. Malaysia is among the first nation in the world16 to approve the use of ravidasvir, a new pan-genotypic, second-generation inhibitor of hepatitis C virus of the NS5A protein.17 It is cost-effective alternative therapy for chronic hepatitis C infection. It is hoped that the new treatment can provide better treatment accessibility among opioid dependents who are hepatitis C positive.
In the present study, associations of hepatitis C infection with the methadone dosage or the highest dose required were not identified, probably owing to a wide range of confounders. Nonetheless, hepatitis C reactivity has been reported to affect the dosage required, as the liver, which is the primary target organ for hepatitis C infection, is also the main organ for metabolism of methadone. In addition, hepatitis C virus has been reported to affect the plasma concentration of S-methadone metabolite.18
Heroin was the most commonly used substance, followed by kratom. Heroin is a type of opioid used for its euphoric effects, commonly taken via injection or inhalation.19 Kratom has been used as herbal medicine among locals; it is a μ-opioid agonist with stimulant-like effects, typically taken as drink beverage. Younger people often mix kratom with other harmful substances (mosquito coil, cola, and cough syrup) into cocktails.20,21 There is a trend toward stimulants abuse among the younger population, probably owing to easier accessibility and cheaper price.22,23
The weak positive correlation between methadone dose and frequency of defaulting treatments suggests that patients who were on higher dose had a higher rate of defaulting treatment. This is concerning as they might revert to injectable opioids to aid addiction. Compliance to MMT should be reinforced to ensure optimal use of governmental resources.
No predictor for illicit drug abstinence was identified. Further studies on factors that affect treatment retention and complete abstinence of drug use during MMT are warranted to ensure optimal use of resources for the population of interest.23,24
Conclusion
Among our patients, MMT for opioid dependents cannot sufficiently curb illicit drug use, and there is a shift toward stimulants abuse.
Contributors
All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability
All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics approval
The study was approved by the Medical Research and Ethical Committee of the Ministry of Health Malaysia (reference: NMRR-21-206-58561).
References
- World Health Organization. Data and Statistics. 2021. https://www. euro.who.int/en/health-topics/disease-prevention/illicit-drugs/data- and-statistics
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736-88. Crossref
- Singh J, Gupta P. Drug addiction: current trends and management. Int J Indian Psychol 2017;5:186-201. Crossref
- Degenhardt L, Whiteford HA, Ferrari AJ, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet 2013;382:1564-74Crossref
- Wickersham JA, Marcus R, Kamarulzaman A, Zahari MM, Altice FL. Implementing methadone maintenance treatment in prisons in Malaysia. Bull World Health Organ 2013;91:124-9. Crossref
- Lysaker PH, Davis LW, Warman DM, Strasburger A, Beattie N. Stigma, social function and symptoms in schizophrenia and schizoaffective disorder: associations across 6 months. Psychiatry Res 2007;149:89-95Crossref
- Cheng CM, Chang CC, Wang JD, Chang KC, Ting SY, Lin CY. Negative impacts of self-stigma on the quality of life of patients in methadone maintenance treatment: the mediated roles of psychological distress and social functioning. Int J Environ Res Public Health 2019;16:1299. Crossref
- Sun HM, Li XY, Chow EP, et al. Methadone maintenance treatment programme reduces criminal activity and improves social well-being of drug users in China: a systematic review and meta-analysis. BMJ Open 2015;5:e005997. Crossref
- Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Setting. Geneva: World Health Organization; 2009.
- World Health Organization Model List of Essential Medicines. Geneva: World Health Organization; 2019.
- Lemeshow S, Hosmer DW Jr, Klar J, Lwanga SK. Adequacy of sample size in health studies. 1st ed. Wiley; 1990.
- Fonseca F, Gratacòs M, Escaramís G, et al. Response to methadone maintenance treatment is associated with the MYOCD and GRM6 genes. Mol Diagn Ther 2010;14:171-8. Crossref
- Ripanda AS, Srivastava BBL, Vuai SH, Nyundo AA. Prevalence and factors associated with continual opioid use among patients attending methadone clinic at Mwananyamala Hospital, Dar es Salaam, Tanzania. Forensic Sci Int Rep 2019;1:100037. Crossref
- Axley P, Ahmed Z, Ravi S, Singal AK. Hepatitis C virus and hepatocellular carcinoma: a narrative review. J Clin Transl Hepatol 2018;6:79-84. Crossref
- Suan MAM, Said SM, Azman AZF, Hassan MRA. A narrative review of natural history, epidemiology and risk factors for hepatitis C infection. Pertanika J Sci Tech 2019;27:1341-59.
- Bala Krishnan D. Malaysia gives conditional approval to Hepatitis C drug Ravida. New Straits Times 2021. https://api.nst.com.my/ news/nation/2021/06/698607/malaysia-gives-conditional-approval- hepatitis-c-drug-ravida
- Cheong MWL, Piedagnel JM, Khor SK. Ravidasvir: equitable access through an alternative drug development pathway. Lancet Glob Health 2021;9:e1496-7. Crossref
- Wu SL, Wang SC, Tsou HH, et al. Hepatitis C virus infection influences the S-methadone metabolite plasma concentration. PLoS One 2013;8:e69310. Crossref
- Rook EJ, van Ree JM, van den Brink W, et al. Pharmacokinetics and pharmacodynamics of high doses of pharmaceutically prepared heroin, by intravenous or by inhalation route in opioid-dependent patients. Basic Clin Pharmacol Toxicol 2006;98:86-96. Crossref
- Tungtananuwat W, Lawanprasert ST. Fatal 4×100; home-made kratom juice cocktail. J Health Res 2010;24:43-7.
- Khalid K, Ku Md Saad S, Soelar SA, Mohamed Yusof Z, Warijo O. Exploring adolescents’ practice and perspective on the use and misuse of kratom in northwest Malaysia. J Ethn Subst Abuse 2021:1-12Crossref
- Ellis MS, Kasper ZA, Cicero TJ. Twin epidemics: the surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend 2018;193:14-20. Crossref
- Davidson C. Developing treatments for stimulant abuse: a brief overview. East Asian Arch Psychiatry 2016;26:52-9.
- Ren Q, Ma M, Hashimoto K. Current status of substance abuse in East Asia and therapeutic prospects. East Asian Arch Psychiatry 2016;26:45-51.