East Asian Arch Psychiatry 2024;34:82-86 | https://doi.org/10.12809/eaap2422
ORIGINAL ARTICLE
Abstract
Background: We investigated the prevalence of restless legs syndrome (RLS) among Jordanian medical students and its association with stress, anxiety, smoking, caffeine use, study habits, and academic performance.
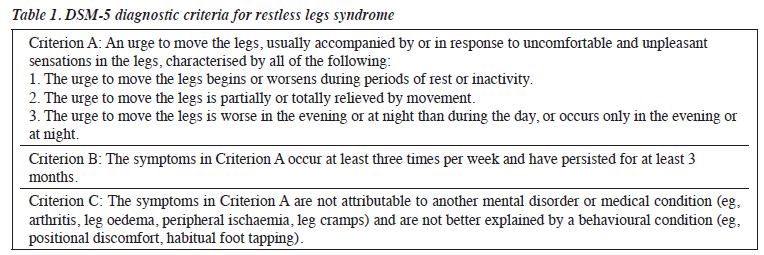
Methods: A cross-sectional study was conducted between November 2023 and January 2024 among medical students in the Jordanian public universities. Participants were selected to complete a questionnaire (based on the DSM-5 diagnostic criteria for RLS) through convenience and snowball sampling.
Results: Among the 215 participants, 11 men and 13 women met the diagnostic criteria for RLS based on their questionnaire responses; the prevalence of RLS was 11.2%. Among these 24 participants, 66.7% reported worsened symptoms during examination periods; 79.1% reported worsened symptoms when experiencing daytime stress; 62.5% reported improved symptoms following physical activity; 66.7% reported that RLS symptoms affected sleep quality; and 45.8% reported having a concomitant anxiety disorder. Meeting the criteria for RLS was not associated with sex, academic stage (basic vs clinical), smoking status, or academic performance.
Conclusion: RLS is not uncommon among medical students in Jordan. Greater awareness of RLS is needed for prompt diagnosis and treatment to prevent associated negative impacts.
Tariq Al-Hunaiti, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Laith Ashour, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Baraah Jamal, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Lina A Abu Sirhan, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Rabie Iqnaibi, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Reem Abdel Hafez, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Noor Alrawajfeh, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Mohammad Alsouri, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Khaled Funjan, Department of Basic Medical Sciences, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
Address for correspondence: Dr Laith Ashour, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, 19117, Jordan. Email: laithashour100@gmail.com
Submitted: 25 April 2024; Accepted: 12 June 2024
Medical education is both academically and emotionally demanding, which may have a negative impact on the mental health of medical students, potentially leading to depression and anxiety.1 In a meta-analysis, the global prevalences of depression and anxiety among medical students are 28% and 33.8%, respectively.2 The prevalence of irritable bowel syndrome among medical students ranges from 9.3% to 35.5%, which is higher than that of the general population, probably owing to the stressful learning environment.3
Restless legs syndrome (RLS) is characterised by an uncomfortable need to move the legs or walk while resting and is often worse at night. It may be idiopathic or secondary to pregnancy or systemic disorders such as iron deficiency and chronic renal insufficiency.4 The presence of a family history is common.4 The pathogenesis of RLS involves dopaminergic dysfunction in the central nervous system. Clinical evaluation includes a thorough history taking, physical examination, and blood tests for ferritin and transferrin saturation.4 In a study of 300 medical students in Karachi, 24 (8%) had RLS and it was more common in females.5 Among medical students in Turkey, those with RLS reported poorer sleep quality,6 which may affect academic performance and be associated with mood disorders.
Awareness of RLS may help students to access appropriate behavioural or pharmacological treatments. We aimed to determine the prevalence of RLS among Jordanian medical students and its association with stress, anxiety, smoking, caffeine use, study habits, and academic performance.
Methods
A cross-sectional study was conducted between November 2023 and January 2024 among medical students in the Jordanian public universities (ie, University of Jordan, Al- Balqa Applied University, Hashemite University, Mutah University, Jordan University of Science and Technology, and Yarmouk University). Participants were selected to complete a questionnaire through convenience and snowball sampling; as such, those who believed they had RLS were more likely to participate.
The validity of the questionnaire was initially assessed in 15 students. Minor changes were made to improve question comprehension and the speed of completing the questionnaire, thereby reducing the number of incomplete responses. Based on a previous study in Turkey,6 an estimated sample size of 214 students was required, assuming a margin of error of 5%, a significant level of 0.05, and a response distribution of 16.9%.
Links to the questionnaire were distributed through Facebook groups, and data on demographics (eg, age, sex, academic year, and university), academic performance, and smoking status were collected using the Google Forms. Questions regarding RLS symptoms were based on DSM-5 diagnostic criteria (Table 1) and required binary yes/no responses. For those who met the criteria for RLS, additional questions were asked regarding family history of RLS symptoms, the effect of RLS on anxiety, the presence of other anxiety disorders (such as panic and generalised anxiety disorders), and the effects of potential exacerbating factors (such as examinations, stress, periods of sitting, and caffeine consumption) on RLS symptoms. Responses regarding potential exacerbating factors were measured using a five-point Likert scale, ranging from strongly agree to strongly disagree.
Data were analysed using the JASP software (version 0.18; University of Amsterdam, the Netherlands). Associations of RLS symptoms with sleep quality, academic performance, daytime mood, and daytime productivity were assessed using the Pearson Chi-squared test or Fisher’s exact test. A p value of <0.05 was considered statistically significant.
Results
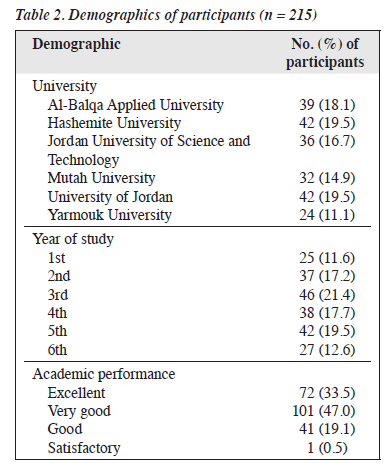
In total, 120 women and 95 men (mean age, 20.7±1.7 years) were included (Table 2); 50.2% were in the first three academic years and the remaining were in the clinical practice years; 85.1% were non-smokers. Among the 215 participants, 122 (56.7%) reported having a frequent urge to move their legs, along with uncomfortable sensations in the legs. However, only 11 men and 13 women met the diagnostic criteria for RLS based on their questionnaire responses; the prevalence of RLS was 11.2%.
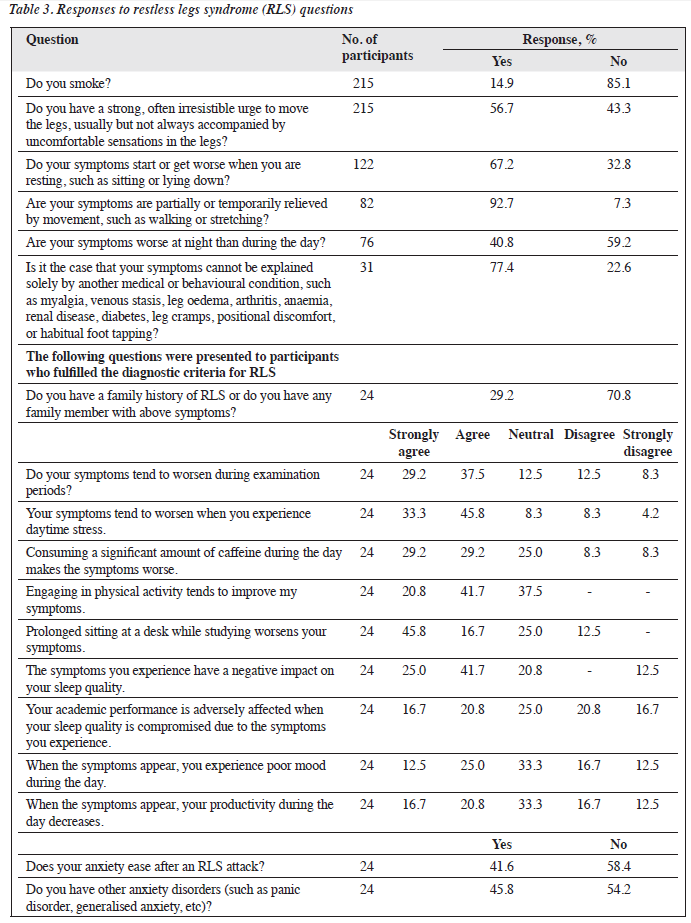
Among the 24 participants who met the criteria for RLS, 66.7% reported worsened symptoms during examination periods; 79.1% reported worsened symptoms when experiencing daytime stress; 62.5% reported worsened symptoms during prolonged periods of sitting at a desk; 62.5% reported improved symptoms following physical activity; 66.7% reported that RLS symptoms affected sleep quality; 37.5% reported that reduced sleep quality affected their academic performance; 37.5% reported that RLS symptoms affected their mood and productivity; 41.6% reported a reduction in anxiety after an RLS attack; and 45.8% reported having a concomitant anxiety disorder (Table 3). Meeting the criteria for RLS was not associated with sex (p = 0.83), academic stage (basic vs clinical) [p = 0.19], smoking status (p = 0.37), or academic performance (p = 0.27).
Discussion
The prevalence of RLS among 215 Jordanian medical students was 11.2%, with a slight female predominance. Although there are variations among different countries and populations, the prevalence of RLS ranges from 5% to 10%.7-11 Among medical students, the prevalence was 11.8% in Egypt12 and 8% in Karachi5; both studies also reported a female predominance. The prevalence was 10.25% among medical school faculty members in Brazil,13 11.1% among primary care populations in five Western countries,14 9%
among university students in Slovakia,15 and 8.4% among a middle-aged Saudi population, with a male predominance, which was attributed to the higher rates of smoking and diabetes among men.16 A study of Japanese adults also reported a male predominance.17
Medical students are prone to high stress levels associated with multiple academic requirements, frequent difficult examinations, and broad extensive curricula.18-21 In our study, RLS symptoms were reported to increase in severity during examination periods and times of daytime stress, consistent with a study of Turkish adolescents that found symptoms associated with heavy training or playing sports during the day.22
Smoking is an exacerbating factor for RLS,5,11,16,23 although this was not found to be significant in our study and other studies.13,24 Prolonged sitting is also a potential exacerbating factor; patients experience RLS symptoms during extended periods of sitting in meetings or while studying.22,24,25 RLS has been reported to affect quality of life.26-29 Adolescents with moderate-to-severe RLS exhibit a notable negative mood and lack of energy.22 Negative effects on mood are the most common issue (50%).28 Furthermore, RLS is considered a prevalent sleep disorder.7 RLS can cause sleep disturbance and lead to daytime sleepiness, impaired concentration, and low mood.14,29 60% to 70% of patients with RLS identified sleep disturbance as their main reason for seeking treatment.30,31 The Epworth Sleepiness Scale has been used to evaluated the impact of RLS on daytime somnolence.32 Individuals with RLS are prone to various sleep disturbances.14,28,33,34 In our study, RLS was not associated with academic performance. However, chronic RLS was associated with sleep deprivation and poor academic performance among medical students in Turkey.35 In epidemiological studies, patients with RLS were at higher risk of experiencing depression and anxiety disorders.36 This is similar to other studies that found patients with RLS more likely to have comorbid anxiety and depression.37,38
Patients with RLS who have mild or moderate symptoms are recommended to try non-pharmacological treatments. Because sitting for prolonged periods exacerbates symptoms, taking breaks to walk or exercise may help.39 For sleep-related symptoms, healthy sleep habits including scheduling sleep and wake-up hours are recommended. Cognitive behavioural therapy for insomnia may be indicated if the symptoms are severe.40 Furthermore, adequate psychological support for students should be provided. In addition, mental-alerting activities (such as video games and puzzle games) and avoidance of substances or medications that may exacerbate RLS symptoms are recommended.41
Conclusion
RLS is not uncommon among medical students in Jordan. Greater awareness of RLS is needed for prompt diagnosis and treatment to prevent associated negative impacts.
Contributors
All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics approval
This study was approved by the ethics committee of the Faculty of Medicine, Al-Balqa Applied University (reference: 2024-0012). The participants provided written informed consent for all treatments and procedures and for publication.
References
- Quek TT, Tam WW, Tran BX, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health 2019;16:2735. Crossref
- Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ 2016;50:456-68. Crossref
- Ibrahim NK. A systematic review of the prevalence and risk factors of irritable bowel syndrome among medical students. Turk J Gastroenterol 2016;27:10-6. Crossref
- Gossard TR, Trotti LM, Videnovic A, St Louis EK. Restless legs syndrome: contemporary diagnosis and treatment. Neurotherapeutics 2021;18:140-55. Crossref
- Ishaq M, Riaz SU, Iqbal N, et al. Prevalence of restless legs syndrome among medical students of Karachi: an experience from a developing country. Sleep Disord 2020;2020:7302828. Crossref
- Sarıaydın M, Günay E, Ünlü M. Frequency of restless legs syndrome and relationship between depression, anxiety and sleep quality among medical school students [in Turkish]. Tuberk Toraks 2018;66:217-23. Crossref
- Dauvilliers Y, Winkelmann J. Restless legs syndrome: update on pathogenesis. Curr Opin Pulm Med 2013;19:594-600. Crossref
- Innes KE, Selfe TK, Agarwal P. Prevalence of restless legs syndrome in North American and Western European populations: a systematic review. Sleep Med 2011;12:623-34. Crossref
- Ohayon MM, O’Hara R, Vitiello MV. Epidemiology of restless legs syndrome: a synthesis of the literature. Sleep Med Rev 2012;16:283-95. Crossref
- Ergin N, Kılıç BB, Ergin A, Varlı S. Sleep quality and related factors including restless leg syndrome in medical students and residents in a Turkish university. Sleep Breath 2022;26:1299-307. Crossref
- 1 Picchietti MA, Picchietti DL. Restless legs syndrome and periodic limb movement disorder in children and adolescents. Semin Pediatr Neurol 2008;15:91-9. Crossref
- Shalash AS, Elrassas HH, Monzem MM, Salem HH, Abdel Moneim A, Moustafa RR. Restless legs syndrome in Egyptian medical students using a validated Arabic version of the Restless Legs Syndrome Rating Scale. Sleep Med 2015;16:1528-31. Crossref
- Haggstram FM, Bigolin AV, Assoni AS, et al. Restless legs syndrome: study of prevalence among medical school faculty members. Arq Neuropsiquiatr 2009;67:822-6. Crossref
- Hening W, Walters AS, Allen RP, Montplaisir J, Myers A, Ferini- Strambi L. Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: the REST (RLS epidemiology, symptoms, and treatment) primary care study. Sleep Med 2004;5:237-46. Crossref
- Minár M, Valková P, Valkovič P. Prevalence and impact of restless legs syndrome in university students. Mov Disord 2013;28:1157-8. Crossref
- Wali SO, Abaalkhail B. Prevalence of restless legs syndrome and associated risk factors among middle-aged Saudi population. Ann Thorac Med 2015;10:193-8. Crossref
- Kageyama T, Kabuto M, Nitta H, et al. Prevalences of periodic limb movement-like and restless legs-like symptoms among Japanese adults. Psychiatry Clin Neurosci 2000;54:296-8. Crossref
- Behere SP, Yadav R, Behere PB. A comparative study of stress among students of medicine, engineering, and nursing. Indian J Psychol Med 2011;33:145-8. Crossref
- Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. PeerJ 2015;3:e840. Crossref
- Saipanish R. Stress among medical students in a Thai medical school. Med Teach 2003;25:502-6. Crossref
- Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ 2007;7:26. Crossref
- Yilmaz K, Kilincaslan A, Aydin N, Kor D. Prevalence and correlates of restless legs syndrome in adolescents. Dev Med Child Neurol 2011;53:40-7. Crossref
- Fereshtehnejad SM, Rahmani A, Shafieesabet M, et al. Prevalence and associated comorbidities of restless legs syndrome (RLS): data from a large population-based door-to-door survey on 19176 adults in Tehran, Iran. PLoS One 2017;12:e0172593. Crossref
- Ibrahim M, Zahoor IA, Javed AN, Rana AA, Ain NU, Rashid M. Incidence of restless leg syndrome among medical school faculty members. Pak Biomed J 2022;5:36-40. Crossref
- Allen RP, Earley CJ. Restless legs syndrome: a review of clinical and pathophysiologic features. J Clin Neurophysiol 2001;18:128-47. Crossref
- Almutairi AH, Alatawi AA, Binsufayan SA. Evaluation of prevalence and associated factors of restless leg syndrome among medical students at University of Tabuk, 2017. Egypt J Hosp Med 2018;70:1440-4.Crossref
- Bogan RK, Cheray JA. Restless legs syndrome: a review of diagnosis and management in primary care. Postgrad Med 2013;125:99-111 Crossref
- Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med 2005;165:1286-92. Crossref
- Garcia-Borreguero D. Time to REST: epidemiology and burden. Eur J Neurol 2006;13 Suppl 3:15-20. Crossref
- Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med 2003;4:101-19. Crossref
- Rijsman R, Neven AK, Graffelman W, Kemp B, de Weerd A. Epidemiology of restless legs in The Netherlands. Eur J Neurol 2004;11:607-11. Crossref
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-5. Crossref
- Saletu B, Anderer P, Saletu M, Hauer C, Lindeck-Pozza L, Saletu- Zyhlarz G. EEG mapping, psychometric, and polysomnographic studies in restless legs syndrome (RLS) and periodic limb movement disorder (PLMD) patients as compared with normal controls. Sleep Med 2002;3 Suppl:S35-42. Crossref
- Ulfberg J, Nyström B, Carter N, Edling C. Restless legs syndrome among working-aged women. Eur Neurol 2001;46:17-9. Crossref
- Yon MI, Akdeniz G, Sen AB, Bozkus E, Yoldas TK. Prevalence of restless legs syndrome among medical students and the effect of disease on academic performance. Ann Med Res 2020;27:74-8. Crossref
- Becker PM, Sharon D. Mood disorders in restless legs syndrome (Willis-Ekbom disease). J Clin Psychiatry 2014;75:e679-e694. Crossref
- Winkelmann J, Prager M, Lieb R, et al. “Anxietas tibiarum”. Depression and anxiety disorders in patients with restless legs syndrome. J Neurol 2005;252:67-71. Crossref
- Lee HB, Hening WA, Allen RP, et al. Restless legs syndrome is associated with DSM-IV major depressive disorder and panic disorder in the community. J Neuropsychiatry Clin Neurosci 2008;20:101-5.Crossref
- Aukerman MM, Aukerman D, Bayard M, Tudiver F, Thorp L, Bailey B. Exercise and restless legs syndrome: a randomized controlled trial. J Am Board Fam Med 2006;19:487-93. Crossref
- Song ML, Park KM, Motamedi GK, Cho YW. Cognitive behavioral therapy for insomnia in restless legs syndrome patients. Sleep Med 2020;74:227-34. Crossref
- Silber MH, Buchfuhrer MJ, Earley CJ, et al. The management of restless legs syndrome: an updated algorithm. Mayo Clin Proc 2021;96:1921-37. Crossref


