East Asian Arch Psychiatry 2024;34:70-3 | https://doi.org/10.12809/eaap2415
ORIGINAL ARTICLE
Abstract
Objectives: This study aimed to compare mental healthcare services for older adults aged ≥65 years among countries in World Psychiatric Association (WPA) Zone 10.
Methods: A culturally sensitive questionnaire was developed and sent to the presidents of national psychiatric associations of the eight countries in WPA Zone 10 (Armenia, Azerbaijan, Belarus, Kazakhstan, Kyrgyzstan, Moldova, Russia, and Uzbekistan).
Results: Psychiatric associations of six countries responded to the questionnaire (Armenia and Moldova did not respond). The prevalence of mental disorders among older adults (aged ≥65 years) varied from 2.6% in Russia (among those aged ≥60 years) to 3.5% in Azerbaijan, 4% in Uzbekistan, 12.1% in Kazakhstan, and 13.8% in Kyrgyzstan (no data were available for Belarus). Specialised gerontopsychiatric care is provided in all six countries, except for Kazakhstan.
Conclusion: The prevalence of mental disorders in older adults differed among countries in WPA Zone. Improving gerontopsychiatric care is a target for healthcare planners in WPA Zone 10.
Oleg Skugarevsky, Belarusian State Medical University, Minsk, Belarus
Nataliia Petrova, Saint Petersburg State University, Saint Petersburg, Russia
Nikolay G Neznanov, VM Bekhterev National Medical Research Center for Psychiatry and Neurology, IP Pavlov First Saint Petersburg State Medical University, Saint Petersburg, Russia
Kuanysh Altynbekov, Republican Scientific and Practical Center of Mental Health, Asfendiyarov Kazakh National Medical University, Almaty, Kazakhstan
Zarifjon Ashurov, Republicаn Speciаlized Scientific-Prаcticаl Medicаl Centre оf Mental Health, Tаshkent Medicаl Аcаdemy, Tаshkent, Uzbekistan
Liliia Panteleeva, Kyrgyz-Russian Slavic University, Kyrgyz State Medical Academy, Bishkek, Kyrgyzstan
Nadir Ismayilov, Azerbaijan Medical University, Baku, Azerbaijan
Tatiana Galako, Kyrgyz-Russian Slavic University, Kyrgyz State Medical Academy, Bishkek, Kyrgyzstan
Jamila Ismayilova, The National Mental Health Center of the Ministry of Health of The Republic of Azerbaijan, Baku, Azerbaijan
Natalia V Semenova, VM Bekhterev National Medical Research Center for Psychiatry and Neurology, Saint Petersburg, Russia
Yekaterina Lyаn, Republican Scientific and Practical Center of Mental Health, Asfendiyarov Kazakh National Medical University, Almaty, Kazakhstan
Egor Chumakov, Saint Petersburg State University, Saint Petersburg, Russia
Address for correspondence: Dr Egor Chumakov, Saint Petersburg State University, Saint Petersburg, Russia. Email: chumakovegor@gmail.com
Submitted: 29 March 2024; Accepted: 8 July 2024
The world population of people aged >65 years was 703 million in 2019 and is expected to increase to 1.5 billion by 2050.1 Population ageing is a challenge for social and healthcare providers, including mental health services, because up to 25% of older people have mental health problems.2 Mental health conditions among older adults are often overlooked and undertreated; many individuals are ashamed or hesitate to seek help owing to the stigma of mental illness.3 This can lead to missed diagnosis and treatment and reduced quality of life. Mental disorders in older adults exacerbate the burden of illness on their microsocial environment, the healthcare system, and society.4,5 The increased demand for psychological services among older adults, particularly with respect to the emotional and psychological difficulties caused by chronic illnesses, is increasingly relevant.6,7 The COVID-19 pandemic was a significant contributor to the increasing mental health difficulties among older adults.8-10 This study aimed to compare mental healthcare services for older adults aged ≥65 years among countries in World Psychiatric Association (WPA) Zone 10.
Methods
The study was initiated by the representative of WPA Zone 10, which comprises eight countries: Armenia, Azerbaijan, Belarus, Kazakhstan, Kyrgyzstan, Moldova, Russia, and Uzbekistan. A culturally sensitive questionnaire was developed and sent to presidents of the national psychiatric associations of the eight countries in WPA Zone 10 between February and March 2023. Only six national psychiatric associations (Azerbaijan, Belarus, Kazakhstan, Kyrgyzstan, Russia, and Uzbekistan) responded and provided data on the prevalence of mental disorders among older adults and mental healthcare services available to them. Diagnoses were based on the ICD-10.
Results
The proportion of older adults varied greatly among the six countries that responded: from 4.8% in Kyrgyzstan to 6.7% in Uzbekistan, 7.7% in Kazakhstan, 15.96% in Belarus, and 16.0% in Russia (data were not available for Azerbaijan). The respective mean life expectancies of men and women, were 64 and 78 years in Belarus, 65.5 and 73.1 years in Kazakhstan, 68 and 76 years in Kyrgyzstan, 67.6 and 77.8 years in Russia, and 71.7 and 75.8 years in Uzbekistan (data were not available for Azerbaijan). The proportion of older people living in social care institutions was 0% in Kazakhstan, 0.2% in Kyrgyzstan, and 0.5% in both Russia and Uzbekistan (data were not available for Belarus and Azerbaijan).
Psychiatric associations of six countries responded to the questionnaire (Armenia and Moldova did not respond). The prevalence of mental disorders among older adults was 3.5% in Azerbaijan, 3.7% in Russia (calculated from the provided rate of 2.6% among those aged ≥60 years), 4% in Uzbekistan, 12.1% in Kazakhstan, and 13.8% in Kyrgyzstan (data were not available for Belarus). Public specialised gerontopsychiatric care was provided in all six countries except Kazakhstan. In Kyrgyzstan, specialised gerontopsychiatric care was mainly provided in private centres, according to the Global Burden of Disease 2019 study.11 In Russia, there were over 1500 gerontological institutions; almost 90% of which were municipal and state institutions; some had gerontopsychiatric units.
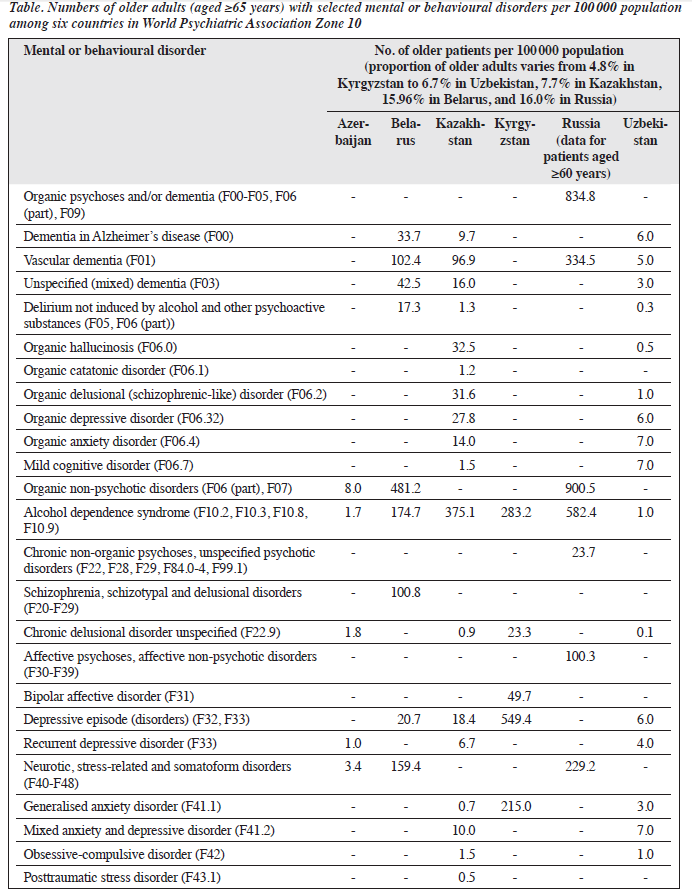
The prevalences of older adults with selected mental and behavioural disorders in Azerbaijan, Belarus, Kazakhstan, Kyrgyzstan, Russia, and Uzbekistan are shown in the Table. Comparisons among countries were challenging owing to the lack of unified approaches to statistical reporting.
Discussion
Among the six countries of WPA Zone 10 that responded to the questionnaire, the proportion of older adults varied greatly, with a mean being 10.23%. Among countries in the WPA Zone 10, the proportion of older adults with mental disorders was <8%, which is lower than that in other parts of the world.3,12,13 However, owing to the lack of data or unified statistical reporting in some countries, it is difficult to estimate the prevalence of each mental and behavioural disorder. It should be noted that the prevalences of affective disorders and vascular dementia stand out. Post-traumatic stress disorder seems to be the most difficult to diagnose, as it was not reported in five out of six countries in the region, despite its lifetime prevalence in older adults can be as high as 5.5%.14
The mental healthcare system for older adults varies considerably across countries of WPA Zone 10. Public specialised gerontopsychiatric care is available in four of the six countries that responded to the questionnaire. The lack of provision of psychiatric care for older people is also relevant in other regions of the world.15 Delays in the diagnosis of mental disorders in older people is common.16 Therefore, it is important to increase access to mental health services and early interventions for older adults.6,17
Consistent with a previous study,18 providing and receiving mental health services among older people in countries of WPA Zone 10 remains challenging. Older people with mental health problems usually require more personal care, more hours of care, and more intensive supervision than older people with other chronic illnesses.19 Unfortunately, there is a lack of evidence to inform the provision of such care for older people with mental health problems (including depression, anxiety, and schizophrenia) other than dementia.
The present study has limitations. Not all countries in the region responded to the questionnaire. The reason why Armenia and Moldova did not respond is not known. Differences in statistical reporting systems between countries preclude detailed comparisons of specific categories. More studies are warranted to identify cultural, economic, organisational, and other factors that affect the prevalence of mental disorders in older adults.
Conclusion
The prevalence of mental disorders in older adults varies significantly among countries in WPA Zone 10. It is beneficial to develop a unified system for assessing the sociodemographics and prevalences of mental disorders in older adults, based on the ICD-11. Improving gerontopsychiatric care is a target for healthcare planners in WPA Zone 10.
Contributors
OS, NP, and EC designed the study. OS, NGN, KA, ZA, LP, NI, TG, JI, NVS, and YL acquired and analysed the data. NP and EC drafted the manuscript. All authors critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics approval
This study did not involve collection or analysis of patients’ personal data.
References
- United Nations, Department of Economic and Social Affairs, Population Division. 2019. World Population Ageing 2019: Highlights (ST/ESA/SER.A/430). United Nations.
- Spasova S, Baeten R, Coster S, Ghailani D, Peña-Casas R, Vanhercke B. Challenges in Long-Term Care in Europe. A Study of National Policies. European Social Policy Network (ESPN), Brussels: European Commission (2018). Accessed 1 June 2023. Available from: https://ec.europa.eu/social/main.jsp?langId=en&catId=1135&newsId=9185&furtherNews=yes&furtherNews=yes.
- World Health Organization. Mental health of older adults. Accessed 1 March 2024. Available from: https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults.
- Gontijo Guerra S, Berbiche D, Vasiliadis HM. Changes in instrumental activities of daily living functioning associated with concurrent common mental disorders and physical multimorbidity in older adults. Disabil Rehabil 2021;43:3663-71. Crossref
- Neumann L, Dapp U, Jacobsen W, van Lenthe F, von Renteln-Kruse W. The MINDMAP project: mental well-being in urban environments: design and first results of a survey on healthcare planning policies, strategies and programmes that address mental health promotion and mental disorder prevention for older people in Europe. Z Gerontol Geriatr 2017;50:588-602. Crossref
- Abdi S, Spann A, Borilovic J, de Witte L, Hawley M. Understanding the care and support needs of older people: a scoping review and categorisation using the WHO international classification of functioning, disability and health framework (ICF). BMC Geriatr 2019;19:195. Crossref
- Ho CSH, Wong SY, Chiu MM, Ho RCM. Global prevalence of elder abuse: a meta-analysis and meta-regression. East Asian Arch Psychiatry 2017;27:43-55.
- Webb L. COVID-19 lockdown: a perfect storm for older people’s mental health. J Psychiatr Ment Health Nurs 2021;28:300. Crossref
- van Tilburg TG, Steinmetz S, Stolte E. Loneliness and mental health during the COVID-19 pandemic: a study among Dutch older adults. J Gerontol B Psychol Sci Soc Sci 2021;76:e249-e255. Crossref
- Louie LLC, Chan WC, Cheng CPW. Suicidal risk in older patients with depression during COVID-19 pandemic: a case-control study. East Asian Arch Psychiatry 2021;31:3-8. Crossref
- Global Burden of Disease 2019 study. Accessed 1 June 2023. Available from: https://ghdx.healthdata.org/gbd-2019.
- World report on ageing and health. 2015. Accessed 1 June 2023. Available from: https://www.who.int/ageing/events/world-report- 2015-launch/en/.
- Ausín B, Muñoz M, Santos-Olmo AB, Pérez-Santos E, Castellanos MA. Prevalence of mental disorders in the elderly in the community of Madrid: results of the Mentdis_ICF65+ Study. Span J Psychol 2017;20:E6. Crossref
- Pless Kaiser A, Cook JM, Glick DM, Moye J. Posttraumatic stress disorder in older adults: a conceptual review. Clin Gerontol 2019;42:359-76. Crossref
- Andreas S, Dehoust M, Volkert J, et al. Affective disorders in the elderly in different European countries: results from the MentDis_ ICF65+ study. PLoS One 2019;14:e0224871. Crossref
- Aakhus E, Granlund I, Odgaard-Jensen J, Oxman AD, Flottorp SA. A tailored intervention to implement guideline recommendations for elderly patients with depression in primary care: a pragmatic cluster randomised trial. Implement Sci 2016;11:32. Crossref
- Wong MMC, Chan CF, Li SW, Lau YM. Six-month follow-up of cognitive impairment and depressive symptoms in late-onset depression. East Asian Arch Psychiatry 2015;25:146-9.
- McKay R, Jackson K, Stevens J. Implementing recovery-oriented practice in older people’s mental health services: the NSW experience. Aust Health Rev 2022;46:426-31. Crossref
- Newbould L, Tucker S, Wilberforce M. Enabling older people with mental health needs to engage with community social care: a scoping review to inform a theory of change. Health Soc Care Community 2022;30:1286-306. Crossref


